It’s two years since the world declared war on COVID. The causative virus, SARS-CoV-2, has proved tenacious and shifting. We’ve begun to talk about living with the virus rather than eradicating it. What will this mean and what are the relative risks of carrying out different activities?
Will vaccines continue to provide protection?
The latest strain (Omicron) is said to cause 'mild' COVID, but a big reason for this is that vaccines - in those who received a course and mounted a normal immune response - have blunted its deadly impact. Omicron is probably more deadly than the original wild-type variant, but the population is now better protected.
Importantly, being vaccinated doesn’t stop you catching and spreading COVID; it just reduces the severity of illness in most people. As we’ve let our guard down, case rates have skyrocketed. A disease with a low mortality rate affecting several million people will kill more people than a disease with a higher mortality rate that only affects a few thousand.
People with compromised immune systems (for example, anyone with a transplant, on chemotherapy, or taking steroids), and anyone who remains unvaccinated for any reason, remain at risk of severe disease and possible fatal outcome. Hence, while vaccination is important, it’s only our first line of defence.
How do different environments affect the spread of COVID?
Step two in living with COVID is to attend to air quality, since the virus spreads mostly in tiny invisible particles suspended in the air.
Droplets (for example, in coughs and sneezes) don’t travel far before falling to the ground or onto surfaces (visible droplets above 100 microns in diameter generally travel up to two metres, but smaller droplets, invisible to the naked eye, are disproportionately slowed by air resistance so travel less than one metre - though a powerful sneeze can send them farther).
Airborne particles are, by definition, much lighter, so they will spread throughout an enclosed space - a room, a car or a train carriage, for example - and can remain in the air for up to four hours after being exhaled.
Read more about coronavirus:
- COVID-19: What is the future of variants after Omicron?
- mRNA vaccines: How COVID jab tech will teach our bodies to kill cancer
This is why ventilation (e.g. opening windows wide to get a through-draught, or using extractor fans) or filtration, e.g. using high-efficiency-particulate-air (HEPA) filters, is an excellent way of reducing the risk of transmission of SARS-CoV-2. If using ventilation, a good proxy for air quality is the carbon dioxide level, since this gas is present in higher concentration in exhaled air. But if air is cleaned by filtration, the carbon dioxide level does not reflect the air quality.
Step three is to understand how airborne viral particles infect you and take steps to reduce this risk. Air is more likely to contain SARS-CoV-2 particles if the local prevalence of COVID is high. If 1 person in 30 in your town has the virus, for example, the chances are that someone in your gym, your supermarket, your open-plan office, your place of worship, or your child’s class is exhaling the virus into the air right now.
People infected with SARS-CoV-2 are at their most contagious before their lateral flow test turns positive and they become fully symptomatic, so it’s no good just avoiding people who have tested positive or reached the stage of feeling terrible. You must assume that someone, you, perhaps, may be unwittingly infecting the air.
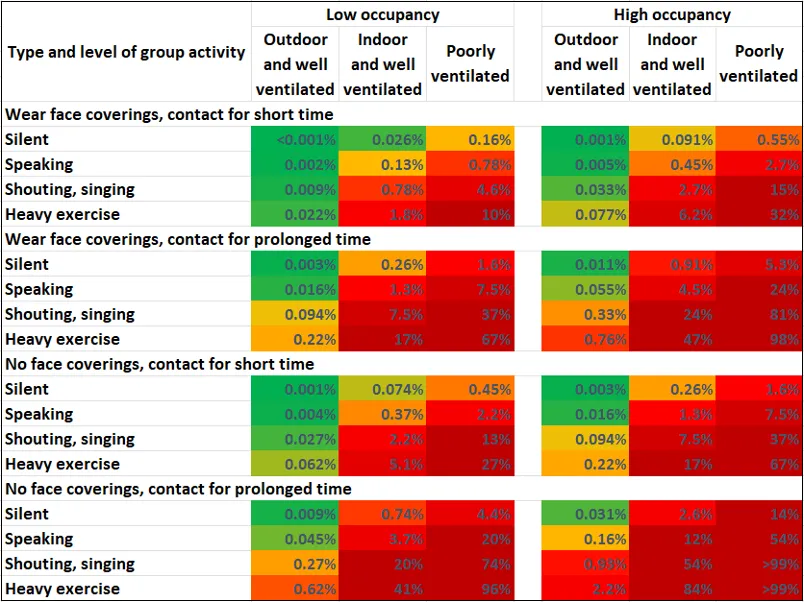
SARS-CoV-2 infection doesn’t usually occur in a one-shot hit but by exposing the inside of the lungs to viral-laden air over minutes or hours. At any given prevalence of COVID-19, the chance of catching the virus is greater the smaller the space, the lower the ventilation, the more people are gathered together, the fewer of them are masking, the more noise they’re making and the longer they stay there.
Take, for example, an indoor space such as a church that measures 30 x 10 metres. Let’s say it is poorly ventilated, less than one air change per hour, and 50 people gather in it for one hour, not wearing face coverings and singing. If approximately 1 in 100 people in the population has COVID-19, the chance of someone catching the disease at this gathering is - depending on other factors such as humidity - 37 per cent.
If, on the other hand, the room is well ventilated, having 10 air changes per hour, and everyone present wears a well-fitting mask, the chance of someone becoming infected drops to below 3 per cent. And if they stay silent, the risk falls to below 0.1 per cent.
To reduce the chance of getting infected, spend as little time as possible in small, enclosed and unventilated spaces, especially crowded ones. Walk rather than take the bus, for example. Shop in small stores early in the morning when they’ve been empty overnight. Hold work meetings by video call or while walking outdoors. If you’re a teacher, send the kids out to play for 10 minutes every hour and throw the windows wide open until they return.
Read more about coronavirus:
- Will we have to live with COVID forever? A virologists explains
- What is the future of variants after omicron?
The closer you are to someone when they exhale, the more likely you are to catch a gulp of their exhaled breath, so staying two metres apart is a sensible precaution. Think halitosis—keep your distance and you’ll avoid the worst. But there’s nothing magical about two metres, especially if you’re sharing air for more than a few minutes.
People emit more viral particles if they’re puffing and panting—when exercising—and also when vocalising - speaking, shouting or singing. So whilst meeting outdoors is generally a safe way to socialise, the exception is the mass event involving a lot of shouting. In such cases, such as music festivals, even outdoor events can be risky.
Should I still wear a mask to lower the spread of infection?
Yes, ideally with a high-quality respirator (FFP2 or FFP3 in Europe, equivalent to N95 and N99 respectively in USA) designed to filter out a high percentage of particles. Your mask or respirator has to fit you snugly to avoid air passing through the gaps. Nobody wants to wear masks everywhere or forever, but we need to be canny and wear them in high-risk environments - indoors, where there are a lot of people and they’re speaking or singing - until the local case rate is low.
Personally, I’ll still be wearing mine on public transport, in the gym, in large stores and in the cinema. But since being shouted at is a high-risk activity, I won’t be confronting people who are not wearing masks, especially if they’re quietly minding their own business.
So what’s the bottom line – what can I do safely?
RED activities - avoid these if you care about not catching COVID:
Going to a pub or restaurant, because almost everyone will be unmasked, sitting close together, and talking.
Going to the gym, because here people will be breathing heavily.
Travelling on public transport, as it is usually poorly ventilated and crowded.
AMBER activities - make a judgement, there’s still a risk:
Shopping in supermarkets, as viral-infected air may linger even if there’s hardly anyone in the store.
Working in an office, though the risk depends on occupancy and ventilation.
GREEN activities - low risk:
Just about anything outdoors.
- Visit the BBC’sReality Checkwebsite atbit.ly/reality_check_or follow them on Twitter@BBCRealityCheck