Researchers say they have discovered a technique that can reverse symptoms of Parkinson’s disease in a mouse model of the disease.
They say the technique may represent a new approach to explore for the treatment of neurodegenerative conditions.
A major goal of regenerative medicine is to replace neurons lost during neurodegenerative disorders and promote the integration of new neurons into brain circuits.
For example, Parkinson’s disease is characterised by a loss of dopaminergic neurons in a region of the brain responsible for reward and movement.
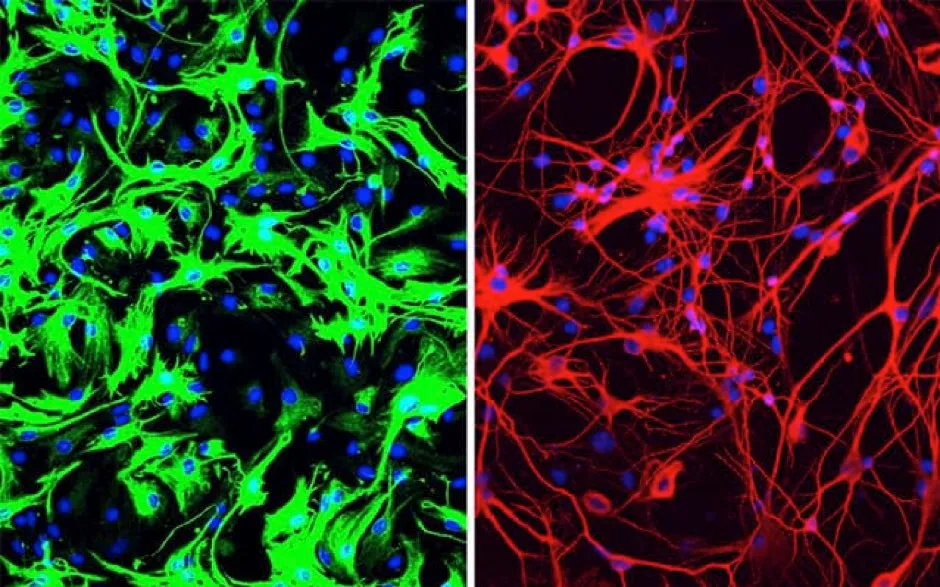
Xiang-Dong Fu and his team at University of California San Diego School of Medicine, say their findings suggest certain brain cells called astrocytes can be turned into functional dopaminergic neurons using a single-step method.
Dr Fu said: “Researchers around the world have tried many ways to generate neurons in the lab, using stem cells and other means, so we can study them better, as well as to use them to replace lost neurons in neurodegenerative diseases.
“The fact that we could produce so many neurons in such a relatively easy way came as a big surprise.”
Read more about Parkinson's disease:
- Parkinson's disease may affect brain before birth
- Prostate drug can 'reduce the signs, symptoms, and complications of Parkinson’s disease'
- Newly-identified gene may help fight dementia risk in Parkinson’s, mice study shows
Astrocytes produce a protein which prevents them from becoming neurons.
Researchers say removing this protein converts them to fully functional neurons that repopulate the lost neuronal circuits, restore dopamine levels and rescue motor deficits in mouse models of Parkinson’s disease.
The study, published in Nature, was conducted in isolated human cells and in mice. But the researchers caution that further research is needed before the approach can be applied to humans.
"It's my dream to see this through to clinical trials, to test this approach as a treatment for Parkinson's disease, but also many other diseases where neurons are lost, such as Alzheimer's and Huntington's diseases and stroke," Dr Fu said. "And dreaming even bigger – what if we could [use this technique] to correct defects in other parts of the brain, to treat things like inherited brain defects?
"I intend to spend the rest of my career answering these questions."
The researchers administered the treatment directly to a part of the mouse’s brain, which is responsible for regulating motor control and reward behaviours, and the part of the brain that typically loses dopamine-producing neurons in Parkinson’s disease.
A control group of mice received mock treatment.
In the treated mice, a small subset of astrocytes converted to neurons, increasing the number of neurons by approximately 30 per cent, the study suggests. Dopamine levels were restored to a level comparable to that in normal mice.
By two different measures of limb movement and response, the treated mice returned to normal within three months after a single treatment. They remained completely free from symptoms of Parkinson’s disease for the rest of their lives.
In contrast, the control mice showed no improvement.
Read more about neurodegenerative diseases:
- Link between brain inflammation and build-up of 'junk' proteins in dementia
- Huntington’s disease can be detected in the brain 24 years before symptoms show
- Staying socially active in middle age could help keep dementia at bay
Professor Tara Spires-Jones of the UK Dementia Research Institute at the University of Edinburgh and deputy director of the Centre for Discovery Brain Sciences, University of Edinburgh, said: “While the principle of this study is remarkable and promising, it is important to note that it was conducted in mice with group sizes from three to eight and there is a long way to go to translate this into a treatment for people.”
Robert Howard, professor of old age psychiatry, at University College London, said the findings were an “extraordinary scientific discovery”.
He added: “This opens up a completely novel avenue for development of treatments to ‘rebuild’ damaged brains in Alzheimer’s and Parkinson’s diseases.
“We will, one day, have effective treatments for these devastating degenerative brain diseases and a specific discovery like this will turn out to have been a pivotal step on the journey – it’s important to bear in mind, however, that this kind of advance rarely translates into safe and effective treatments. Consider the failure of stem cell technologies to help neurological disorders, for example.”
Reader Q&A: How long can the brain live outside the body?
Asked by: James Forbes, by email
The metabolic needs of vertebrate brains are actually fairly simple – mainly oxygen and glucose. These can be supplied by connecting the blood vessels that supply the brain with an artificial blood substitute or by immersing the blood in an artificial cerebro-spinal fluid and oxygenating that directly. Guinea pig, dog and monkey brains have all been kept alive for hours or even days after being removed.
The problem is that, without an attached body, the health of the brain can only be assessed in a fairly basic way. Generally the uptake of oxygen and presence of electrical activity are taken as evidence that the brain is alive. Since there is currently no way to reattach the severed spinal cord, it is very difficult to judge whether the brain is still conscious and fully functioning.
Read more:
