One in two of us will develop cancer in our lifetime. Thanks to advances in diagnosis and treatment, though, more people are surviving cancer than ever. Will this trend continue – and how close are we to finding a cure?
That upward survival trend is likely to continue. But finding a cure? That’s not so easy to answer, for a simple reason: cancer isn’t one single disease but a collection of more than 200, each with unique features. Yet every cancer consists of a mass of abnormal cells, all originating from a single mutated cell that began to divide uncontrollably.
Cell division – one cell dividing to produce two new ones – is essential for growing and maintaining our bodies. Cells that have become worn out or damaged must be replaced. This process is tightly controlled, so that cells are produced only when needed, and in the exact numbers and locations required.
Cancer cells evade those controls and divide chaotically, while also eluding the backup systems that suppress growth and weed out abnormally behaving cells. The result is a tumour. Cancer cells acquire these characteristics through gene mutations.
One important group of genes comprises the proto-oncogenes, which mutate to continuously produce a signal telling cancer cells to divide, becoming oncogenes. Turning off that oncogenic signal stops cancer cells dividing and can even kill them.
That’s the principle underpinning the concept of targeted cancer therapies, a treatment approach in which much progress has been made. Targeted cancer therapies are more effective and have fewer side effects than traditional treatments such as chemotherapy and radiotherapy, and have now been in use for almost 50 years.
The first were hormone therapies used for diseases such as breast and prostate cancer, whose growth depends on the hormones oestrogen and testosterone, respectively. A further step forward came in the 1990s with the development of imatinib (marketed as Glivec).
Developed to inhibit the product of an oncogene present in 99 per cent of chronic myeloid leukaemia (CML) cases, it revolutionised CML treatment. Before imatinib, fewer than three in ten CML patients could expect to survive five years beyond diagnosis. Today, nine in ten do.
The power of big data
Since imatinib, many more targeted therapies have been developed to tackle a diverse range of cancers, with even more undergoing trials. The process of drug discovery has been greatly accelerated by modern genetic techniques that bring the power of big data to cancer research. For example, the Cancer Genome Atlas project contains genetic information on tumours from 11,000 people and 33 types of cancer.
This can be cross-referenced with patient data, enabling deeper insights into how genetic changes drive cancer and its progression, and points towards new treatments by developing new drugs or repurposing old ones. One recent success story is the approval of drugs originally developed for treating malignant melanoma for the treatment of some cases of a type of brain cancer called glioma, after the discovery that their growth was dependent on the same oncogene, BRAF.
This approach offers hope to people diagnosed with rare types of cancers for which no drugs are currently available. Technological advances are also making genome sequencing cheaper and faster, ushering in an era of truly personalised medicine.
In 2022, a team at Stanford University announced that they’d sequenced a full human genome in a record-breaking five hours, and aim to translate that into cancer treatment. In the future, it may become routine to sequence the genome of a patient’s tumour before treatment begins.
Armed with this information, an oncologist will be able to select from an array of targeted drugs to tailor each patient’s treatment exactly, increasing the chance of success. Drug treatments aren’t the only area in which significant progress has been made, though.
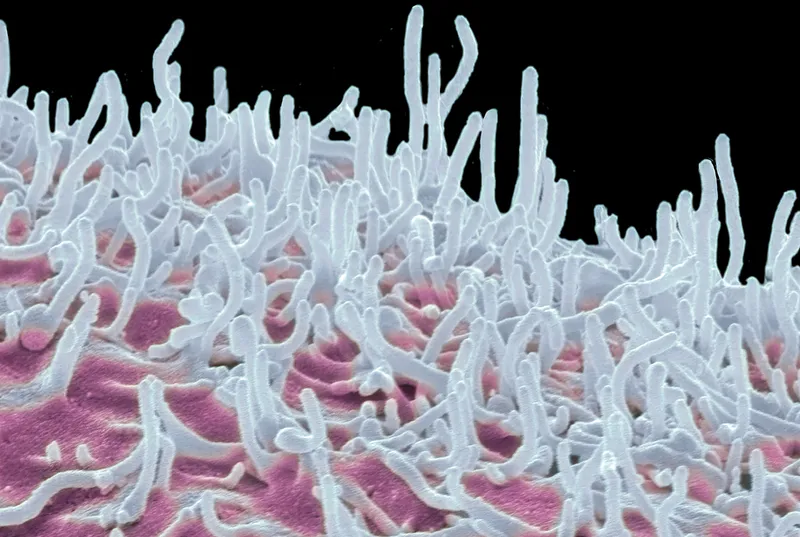
The past decade has seen rapid progress in the use of immunotherapies for cancer. The various types of cancer immunotherapy aim to boost a patient’s immune system so that it’s better able to detect and destroy cancerous cells.
This field is still in its infancy, and we can expect sustained improvements in these treatments over the next decade. Immune checkpoint inhibitors comprise a type of drug that prevents cancers from avoiding detection by the immune system.
They can be incredibly successful as a treatment, but currently work in only some patients. Adoptive cell therapies harvest T cells from patients to make them more effective in fighting cancer.
One very successful example of this is the chimeric antigen receptor T cell (CAR T) therapy. This involves genetically engineering harvested T cells to bind to a specific antigen on the surface of tumour cells.
The modified T cells are then grown in the laboratory before being infused back into the patient’s body to fight the cancer. CAR T cells are very effective against blood cancers, but have been less successful in solid tumours.
This might change with new technological advances that include the ability to switch CAR T cells on and off, timing their activity, and the development of longer-lasting CAR T cells.
Vax on track
Progress has also been made in developing immunisation: vaccinating a patient with cancer antigens to help their immune system detect that cancer. Though the concept has been well established in model systems, translating this into the clinical setting has proved tricky. Every tumour has a unique molecular signature, and a vaccine that works in one patient may not work in another.
mRNA-based vaccines are likely to dramatically change the cancer vaccine landscape. Instead of using a cancer antigen to trigger an immune response, the body is instead provided with instructions (in the form of mRNA) to produce the antigen itself.
This offers several advantages. First, if the molecular signature of a patient’s tumour has been mapped through genome sequencing, the vaccine can be tailored to match. Second, vaccines can be designed to hit multiple targets at once.
Further optimisation, including identifying the best route of delivery, is needed before mRNA cancer vaccines can reach routine clinical use. However, several clinical trials are in progress and showing promising results. Early diagnosis is as important as treatment, if not more so.
The more time a tumour has to grow and evolve, the more difficult treatment becomes. For some cancers, well-established techniques for early diagnosis already exist: national screening programmes for cervical, breast and colorectal cancers, for example. These have led to better outcomes, with more patients surviving.
However, screening tests aren’t available for many cancers. Some, such as pancreatic and lung cancers, are often diagnosed quite late. Artificial intelligence is likely to hold the key to improving cancer diagnosis in the future.
It’s being applied to a wide range of approaches, including tumour image analysis and the development of smart tests to detect the molecular signatures of tumours from traces in the blood. Of course, it would be better if cancer could be prevented altogether. Worldwide, up to 20 per cent of all cancers are caused by chronic infection.
For example, infection with high-risk variants of the human papillomavirus (HPV) can cause a range of cancers including cervical, penile, and head and neck cancers. Similarly, chronic infection with Hepatitis B (HBV) is the main cause of liver cancer.
Vaccines against HPV and HBV are already reducing the incidence of their respective cancers. Through a combination of HPV vaccination and cervical screening, NHS England aims to completely eradicate cervical cancer by 2040.
What about cancers that aren’t caused by infections? Here the concept of cancer interception offers real promise. This involves using a drug or a vaccine to kill cancer cells as they arise, long before they can form a detectable tumour. It can also be used to prevent cancer from recurring in patients who’ve been successfully treated for the disease.
Aromatase inhibitors, a type of hormone therapy used for breast cancer, have been used to prevent disease recurrence for years. More recently they have been licensed by the NHS to prevent breast cancer in women who have a high risk of developing it. The next decade is likely to see further evolution in cancer diagnosis, treatment and prevention.
And although we’re unlikely to ever see a single ‘cure’, the ever-growing arsenal we can access to fight the disease offers new hope to cancer patients everywhere.
Read more: