The coronavirus outcome in the UK “has not been good”, the government’s chief scientific adviser has told MPs.
Sir Patrick Vallance said there will be many factors that determine how well a country responds to the COVID-19 outbreak.He also told the Science and Technology Committee that the virus is likely to be around for a number of years.
Read more about COVID-19:
When asked about the UK’s response to the pandemic, Sir Patrick said: “As [chief medical officer Professor] Chris Whitty has said before, it’s very difficult to know where we stand at the moment. It’s clear that the outcome has not been good in the UK, I think you can be absolutely clear about that.
“It is clear you can see a band of countries that have done less well in the temperate zone. Countries that are very well connected internationally, countries that have got population structures of a certain type.
He added: “There are many factors that are going to play in this as we look and say, ‘what is it that makes some countries having done worse than others?’, and there will be decisions made that will turn out not to have been the right decisions at the time.”
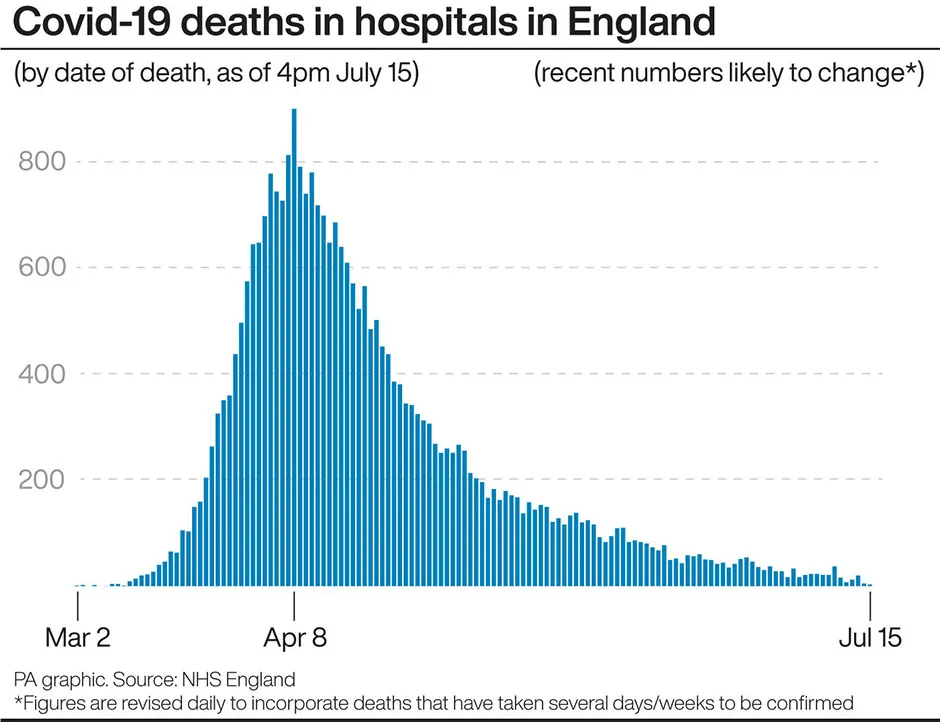
Sir Patrick had previously said 20,000 deaths would be a “good result” in the pandemic, but the latest figures show the UK has seen the deaths rise to more than double that.
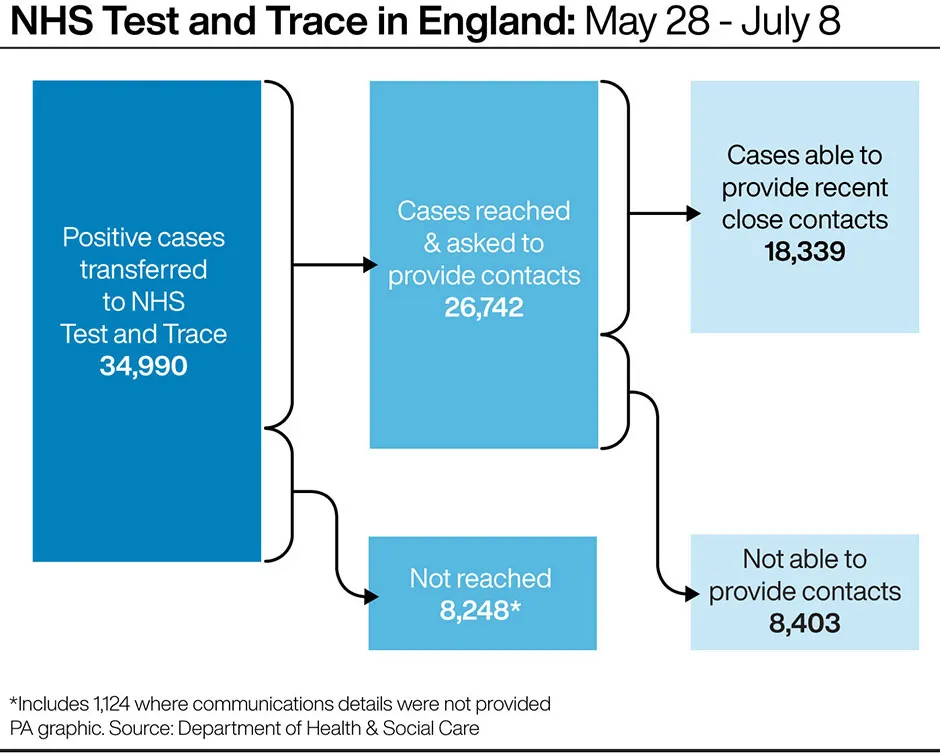
He said that one lesson to learn from the pandemic was the “importance” of data flows.He added: “It would have been absolutely preferable to have much greater testing capacity early on.
“But it’s not just testing, it’s basic information flows around patients in hospitals, around rates of admission, around rates of movement. Those sorts of things are important parts of this as well.”
The committee also heard that what most people refer to when they discuss a second wave of the virus, is actually a re-emergence of the first wave which has been suppressed.
Sir Patrick said that if there is an increase in cases in the winter: “You could argue that is the tail end of the first wave still. And I think it is quite probable that we will see this virus coming back in different waves over a number of years.”
He also told MPs about the risks of lockdown, and that it was “crucially important” that the indirect impact of the lockdown on people’s health was fully understood.
Read the latest coronavirus news:
- Isle of Wight COVID-19 cases 'rapidly declined' after test and trace launch
- Oxford vaccine: Early trials suggest 'double protection' from coronavirus
He said: “I think the chief medical officer has been pretty clear about this, and that is the way this should be looked at… overall excess deaths. If you look at overall excess deaths then you’re looking at the integrated effect of the virus itself with all the other reasons people may have suffered as a result of this.
“We do need to understand the impact of that and it’s very clear that lockdown itself carries risks, and those risks are to both physical health and mental health.”
What is the R number, and why is it relevant to coronavirus?
The reproduction number – often called the R value or R number – is a measure of a disease’s ability to spread. It tells us how many people a single infected person will pass on the disease to.
The R number for COVID-19 that’s being quoted in the media and government briefings is what’s known as the ‘effective’ reproduction number. This value can go up and down.
We can reduce R by making it harder for the disease to spread, by implementing measures such as social distancing, closing restaurants and non-essential shops, and encouraging people to stay at home.
Every disease also has what’s called a ‘basic’ reproduction number, R0, which is the fixed value of R if no measures are put in place. For example, measles is highly contagious, with a R0 as high as 18, while COVID-19 has a R0 of around three.
So if COVID-19 was allowed to spread through the population, an infected person would, on average, give the disease to three other people.
But if all these people are practising physical distancing, then the virus can’t spread so easily and the effective R value goes down.
The crucial thing is to keep R below 1. If we can do this, then the number of new cases dwindles and the outbreak will eventually come to a halt.
Conversely, if R rises above 1, then we run the risk of rapidly escalating case numbers that would require stronger measures to keep the virus under control.
Because of this, R is used by governments to assess how we are doing in our efforts to stop the spread of COVID-19, and to adjust our actions, if needed.
Read more: