Most doctors had accepted by 1900 that bacteria was the cause of many common diseases such as cholera, tuberculosis, typhoid fever and scarlet fever. However, there was still much to learn about the patterns of how these and other diseases spread.
The language of warfare entered medicine with the coming of germs. The body seemed to defend itself against the invaders – sometimes successfully, sometimes not. Two basic theories of immunology matured in the late 19th Century.
One, the brainchild of the Russian Élie Metchnikoff, argued that the white blood cells were key. These circulate in the blood and are found at sites of inflammation. Pus is mostly dead white cells, and Metchnikoff observed them with his microscope. He injected foreign bodies such as thorns and watched as white blood cells attacked bacteria. He called them ‘phagocytes’ and hailed them as the body’s warriors.
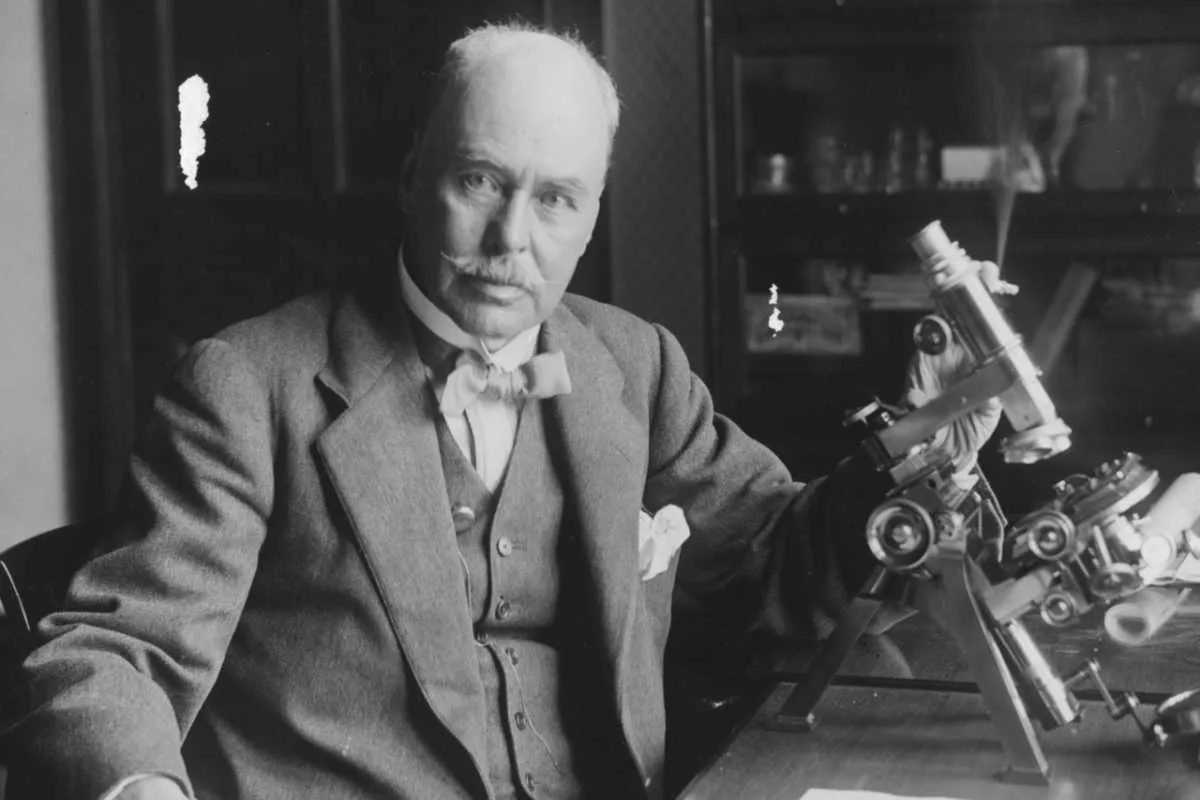
The alternative immunological theory was elaborated by the German scientist Paul Ehrlich, who pioneered the development of experimental pharmacology. Ehrlich argued that the body can produce ‘antibodies’, proteins that fit into foreign bodies (‘antigens’) like a key in a lock.
His chemical theory explained much about infection, including why a first infection often produces immunity against subsequent exposure to the same disease. Smallpox was always used as the example, since people never got it twice.
Read more about the history of disease:
- Robert Koch: how he identified one of the 19th Century's biggest killers
- 10 key scientists in our understanding of disease
- A timeline of discoveries
- The experiment that proved bacteria caused disease
Both theories explained part of the problem and both white blood cells and chemical antibodies are part of modern immunology. But the more scientists learned about the immune system, the more complex it was shown to be.
Another puzzle about the spread of ‘germs’ was elucidated by Robert Koch, who had been instrumental in the original germ theory. He argued that some people could harbour germs without being ill themselves. This ‘carrier state’ was dramatically realised with the case of Mary Mallon, an Irish cook who infected several families with typhoid in New York.
‘Typhoid Mary’ became a cause célèbre as her condition, which was no fault of her own, was diagnosed and she was incarcerated as a danger to the public. She shed typhoid bacilli in faeces and urine, but was not affected by them.
Germ theory afforded public health officials new powers to isolate and contain people against their wills.
Understanding the organisms which cause disease
Bacteria were not the only organisms capable of causing disease. Parasitic worms had long been recognised, and in 1898 Ronald Ross capped five years of research in British India by discovering plasmodia in the salivary glands of mosquitoes. Plasmodia are microorganisms that had first been seen in the blood of humans suffering from malaria by Charles Laveran in 1880.
Ross’s contribution was to show that the parasite was transmitted through the bites of the female Anopheles mosquito. This and the discovery that yellow fever was transmitted through the bites of another genus of mosquito, Aedes, made medical entomology (the study of insects) – at the time an exciting new discipline.
It soon paid off when Charles Nicolle, working in Tunisia, showed that ticks and lice spread typhus. Ross, Laveran and Nicolle each won Nobel Prizes, indicative of the cutting-edge nature of such research.
The infectious agent of yellow fever was a case in point, eventually shown to be caused by a virus. The word was an old one in medicine, and it originally meant simply ‘poison’.
As laboratory methods improved, and scientists began working with a cluster of diseases, such as yellow fever, smallpox and rabies, these agents were shown to pass through the filters that trapped bacteria.

Before these discoveries, Martinus Beijerinck (1851-1931) realised in 1898 that the tobacco mosaic virus (he first called it a ‘virus’) was obliged to multiply in the cells of the plant it infected. This idea, now appreciated as fundamental to our understanding of viruses, was not well received in Beijerinck’s time, since it went against conventional scientific wisdom.
Laboratory scientists eventually came to realise that viruses wouldn’t simply grow in little colonies on Petri dishes like bacteria. Chick embryo cells soon became the medium of choice in laboratories, and as scientists grew more adept at manipulating these tiny particles, they uncovered many viruses that caused human disease. Measles, mumps, chickenpox, smallpox, influenza, polio and the common cold were among the diseases with viral causes.
Need to know
Bacteriophage
A class of viruses that attack bacteria. Understanding how they act proved instrumental in the development of modern molecular biology and genetics.
Prion
A misfolded protein that is so tightly bound that it cannot be broken down by ordinary bodily reactions. It acts as an infectious agent by capturing cellular mechanisms and affecting other proteins.
Vaccine
A substance that stimulates immunity without causing disease. It was named by Louis Pasteur in honour of Edward Jenner’s original use of cowpox (vacca is Latin for cow) to protect against smallpox, a much more serious disease.
Virus
A large group of infectious agents that need the cells of a host in order to replicate. Viruses usually contain either DNA or RNA, coated by a protein shell.
Influenza cast a long shadow on this research, since the 1918-19 Spanish flu pandemic remains the most devastating epidemic in history, killing more than 25 million people worldwide – greater than the casualties in World War I.
Progress was made, however. From 1915 to 1917, Frederick W Twort in London and Félix d’Herelle in Paris discovered what d’Herelle called the ‘bacteriophage’: viruses that infect bacteria. Bacteriophages were initially seen as more curious than important, but over the next three decades, their analysis helped lay the foundations of molecular biology, modern genetics and the structure of DNA.
The electron microscope: seeing is believing
Despite increasing knowledge of viruses during the early decades of the 20th Century, scientists still had no microscope capable of visualising them. This was solved in the early 1930s, when Ernst Ruska and others invented the ‘electron microscope’. This used streams of electrons to provide much higher levels of magnification, and virologists could at last see what they were dealing with.
Patterns of infection confirmed that, with many viral diseases, a single episode leaves the person with lasting immunity. This is why diseases such as mumps, chickenpox and German measles are largely childhood afflictions.
Similarly, vaccines for viruses are frequently more effective than ones for bacterial diseases. Edward Jenner’s cowpox vaccine relied on the cross-immunity that cowpox gave against smallpox, a much more serious disease.

A vaccine for yellow fever was developed in the 1930s, and American scientists worked to find one for polio – probably the most feared disease of young Americans in the middle decades of the 20th Century. After several unsuccessful attempts by various scientists, Jonas Salk announced in 1955 that his vaccine, based on killed polio viruses, was under proper trial.
At about the same time, Albert Sabin introduced his own vaccine. This could be delivered orally, on a lump of sugar, so was much favoured by youngsters, and by 1961 had become the vaccine of choice.
There are effective vaccines for many of the other viral scourges of childhood, as well as the bacterial diseases whooping cough and diphtheria. The capacity to understand and manipulate these germs has made childhood a much safer time in the developed world.
No medical procedure is completely without risk, however, and popular resistance to compulsory vaccination programmes goes back to the 19th Century, when smallpox was the only vaccine available.
Read more about the history of epidemiology:
- Joseph Lister and the grim reality of Victorian surgery
- Viruses: their extraordinary role in shaping human evolution
- How to survive a plague: The story of how activists and scientists tamed AIDS
- The bite that cures: turning venom into medicine
Universal protection is necessary to create the ‘herd immunity’ to protect mass populations. Smallpox vaccination was part of a concerted World Health Organisation (WHO) campaign against the disease, which led to its global eradication by 1980.
The smallpox campaign was run alongside one to eradicate malaria, largely through attempts at mosquito control with DDT. However, the cumulative toxic environmental effects combined with the development of widespread mosquito resistance to the insecticide limited the campaign’s effectiveness. It was quietly abandoned after about a decade.
Efforts to make polio follow smallpox into oblivion have been more successful, although pockets remain where health infrastructure is weak.
The threat of pandemics and emerging infections
These triumphs and failures must be seen beside other diseases. The influenza virus is highly unstable, with new strains demanding vaccines mostly aimed at the current strain. Some of the strains that affect pigs or domestic fowl pose the greatest threat, because they can break the species barrier and threaten human populations. This could cause another global pandemic such as seen in 2020's coronavirus outbreak.
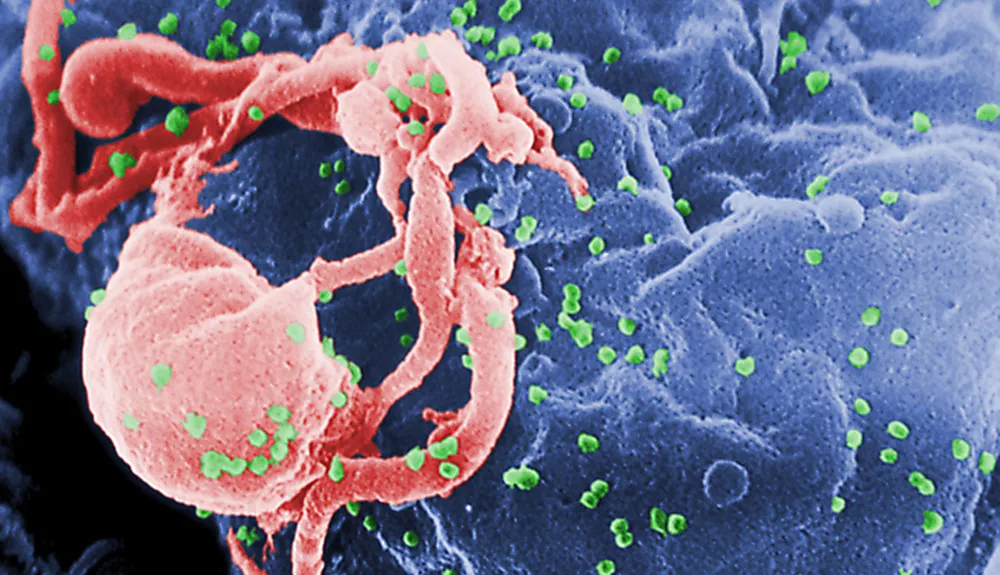
In addition, the modern era has seen the issue of emerging infections. The power of ‘germs’ to inflict suffering and death is nowhere better illustrated than with the identification, in the USA in the early 1980s, of what was first called GRID (gay-related immune deficiency) and then AIDS (Acquired Immunodeficiency Syndrome).
Its early symptoms included fever and sweats, wasting and weakness, a rare kind of tumour (Kaposi’s sarcoma) and infections by organisms that are not normally a threat to human beings. The syndrome was soon discovered in Haiti, in intravenous drug users and in haemophiliacs, and its rapid spread caused concern worldwide.
In 1983 the virus, now called Human Immunodeficiency Virus (HIV), was discovered independently by two groups. The virus was almost certainly first acquired in Africa in the early 20th Century, from chimpanzee meat infected with Simian Immunodeficiency Virus.

It smouldered in humans for several decades until changing social conditions ignited it into an epidemic that spread from Africa to Haiti and then to the US.
HIV has become part of the modern disease landscape. As with several infectious diseases, including syphilis, HIV has changed from an acute to a chronic disease, as the germ and the human body have grown used to one another. As the most-studied virus in history, it has led to innovative drug therapies, although it’s so changeable that a vaccine has proved elusive.
HIV is not the only ‘emerging’ disease to have surfaced in the past half century: Ebola virus, West Nile fever, Legionnaire’s disease, Lyme disease, coronavirus and SARS (Severe Acute Respiratory Syndrome), are also part of our modern world.
In addition, many germs have developed resistance to drugs, and drug-resistant malaria or tuberculosis can act just like a new disease. On top of this, modern hospitals have become seedbeds for MRSA (Methicillin-resistant Staphylococcus aureus).
Half a century ago, many people thought that human beings had largely conquered germs. That optimism was sadly premature.
As if emerging infectious diseases were not enough, a whole new kind of infectious agent has been identified as the cause of scrapie in sheep, bovine spongiform encephalopathy (BSE) in cows and Creutzfeldt-Jakob Disease (CJD) and Kuru in human beings. The ‘agent’, a misfolded protein, was called a prion by Stanley Prusiner in 1982.
Although not living in the conventional sense, prions qualify as ‘infectious’ in their ability to induce other proteins to misfold and thereby become impervious to the normal metabolic processes of proteins. These rogue proteins cause irreversible damage to the nervous system, leading to death within a few months.
At the other end of the spectrum from prions, a bacterium was found in 1982 to be associated with peptic ulcer disease. The work overturned decades of debate about the cause of ulcers and offered a much more effective therapy. It won Robin Warren and Barry Marshall a Nobel Prize for work that theoretically could have been done a century before.
As the war against disease rages on, it’s good to know there are still occasional triumphs.