- Two of the world's fastest supercomputers have been drafted in to analyse libraries of drug compounds that might be able to help develop a coronavirus vaccine.
- Supercomputers are able to analyse vast amounts of data in a matter of days, which would take regular computers months.
- Also being used to study the spread of the virus, as well as analysing its origin and structure.
Supercomputers are playing their part in urgent research into coronavirus, which could help speed up the development of treatments.
The powerful machines are able to process huge amounts of data in a matter of days, compared to months on a regular computer.
This means they can screen libraries of potential antiviral drugs, including those that have already been licensed to treat other diseases.
Read the latest coronavirus news:
- 100 days: what we now know about the coronavirus
- Coronavirus antibody tests: How they work and when we'll have them
- Fingertip-sized coronavirus vaccine 'ready in months'
“We are using the immense power of supercomputers to rapidly search vast numbers of potential compounds that could inhibit the novel coronavirus, and using the same computers again, but with different algorithms, to refine that list to the compounds with the best binding affinity,” said Professor Peter Coveney, from UCL (University College London).
“That way, we are identifying the most promising compounds ahead of further investigations in a traditional laboratory to find the most effective treatment or vaccination for COVID-19.”
Scientists at UCL have access to some of the world’s most powerful supercomputers, as part of a consortium with more than a hundred researchers from across the US and Europe.
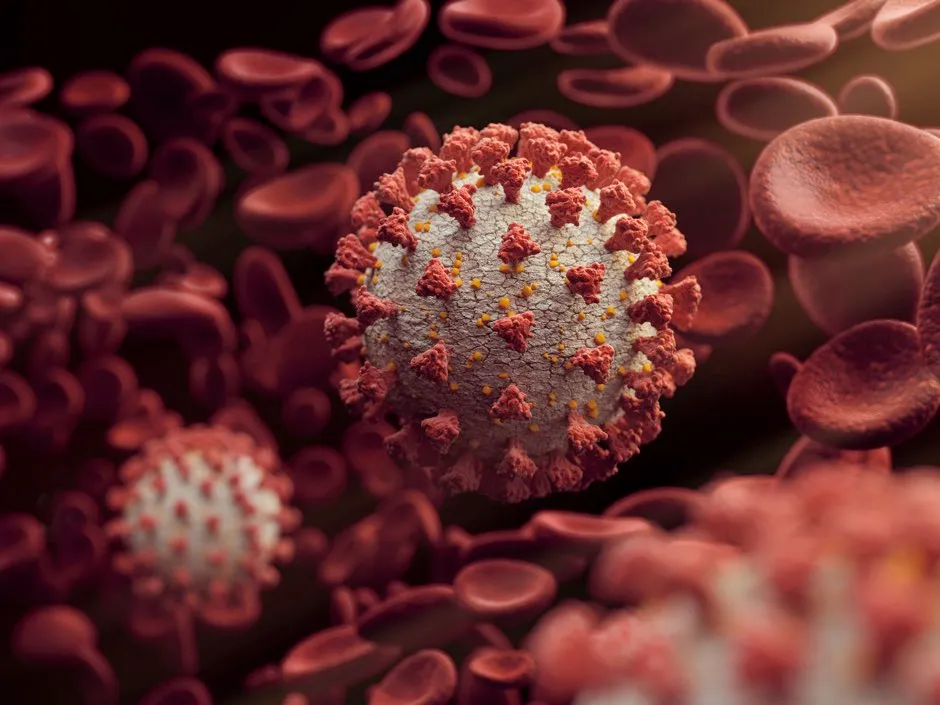
The world’s fastest, Summit, at Oak Ridge National Lab in the US and the world number nine, SuperMUC-NG in Germany, are included, which can analyse libraries of drug compounds to identify those capable of binding to the spikes on the surface of coronavirus, which the virus uses to invade cells, so as to prevent it from infecting human cells.
These machines could help by identifying virus proteins or parts of a protein that stimulate immunity which could be used to develop a vaccine.
They can also study the spread of the virus within communities, as well as analysing its origin and structure, and how it interacts with human cells.
Read more about the coronavirus pandemic:
- Corrupted Blood: what the virus that took down World of Warcraft can tell us about coronavirus
- Big tech and coronavirus: How Google and Facebook could take on the pandemic
- What nature can teach us about friendship in the time of coronavirus
- 10 science-backed tips to help you work from home successfully
“This is a much quicker way of finding suitable treatments than the typical drug development process,” Professor Coveney continued.
“It normally takes pharma companies 12 years and two billion dollars to take one drug from discovery to market but we are rewriting the rules by using powerful computers to find a needle in a haystack in a fraction of that time and cost.”
How do scientists develop vaccines for new viruses?
Vaccines work by fooling our bodies into thinking that we’ve been infected by a virus. Our body mounts an immune response, and builds a memory of that virus which will enable us to fight it in the future.
Viruses and the immune system interact in complex ways, so there are many different approaches to developing an effective vaccine. The two most common types are inactivated vaccines (which use harmless viruses that have been ‘killed’, but which still activate the immune system), and attenuated vaccines (which use live viruses that have been modified so that they trigger an immune response without causing us harm).
A more recent development is recombinant vaccines, which involve genetically engineering a less harmful virus so that it includes a small part of the target virus. Our body launches an immune response to the carrier virus, but also to the target virus.
Over the past few years, this approach has been used to develop a vaccine (called rVSV-ZEBOV) against the Ebola virus. It consists of a vesicular stomatitis animal virus (which causes flu-like symptoms in humans), engineered to have an outer protein of the Zaire strain of Ebola.
Vaccines go through a huge amount of testing to check that they are safe and effective, whether there are any side effects, and what dosage levels are suitable. It usually takes years before a vaccine is commercially available.
Sometimes this is too long, and the new Ebola vaccine is being administered under ‘compassionate use’ terms: it has yet to complete all its formal testing and paperwork, but has been shown to be safe and effective. Something similar may be possible if one of the many groups around the world working on a vaccine for the new strain of coronavirus (SARS-CoV-2) is successful.
Read more:
