Four months since its approval for use in the UK, the Oxford/AstraZeneca vaccine has been administered to tens of millions of people across the country.
However, due to a possible link with rare blood clots, people under 30 will now be offered an alternative coronavirus vaccine (where available) after a recommendation from the UK’s Medicines and Healthcare products Regulatory Agency.
The recommendation came after it was found that after 20 million Oxford/AstraZeneca doses were administered, 79 people who received the jab suffered blood clots, 19 of whom died.
Although concerns have been raised, it’s not yet been confirmed how the vaccine could be linked to these deaths.
However, the development has understandably led to a series of new questions about the jab and its safety.
Does the Oxford/AstraZeneca vaccine cause blood clots?
Although studies are currently examining the small correlation between the Oxford/AstraZeneca vaccine and life-threatening blood clots, there is no definite causal link.
True, the EU regulator’s head of vaccines, Marco Cavaleri previously said there’s a “clear link” between the two. However, the EMA (European Medicines Agency) later clarified they had not discovered a causal connection between the vaccine and blood clots. On Tuesday 6 April they said it had “not yet reached a conclusion and the review is currently ongoing.”
The main cause for concern is that similar ratios of blood clots haven’t been found in people given the Pfizer or Moderna jabs (mRNA vaccines).
“However, it’s possible countries that have been mainly administering these mRNA vaccines, such as the US, just haven’t been looking as hard at this issue – this could change,” says Dr Connor Bamford, virologist at Queen’s University Belfast.
How could the Oxford/AstraZeneca vaccine produce blood clots?
Again, there is no solid evidence that the jab causes blood clots. However, the EMA has proposed one possible explanation. According to the agency, many of the same innate immune responses that fight infection also trigger blood clots in some people.
The Oxford/AstraZeneca vaccine works by generating an immune response to a non-harmful material imitating the coronavirus – the response means the body is ‘trained’ if it attacked by the real thing. However, as all vaccines aim to produce a similar immune response, it is not clear why this would only be an issue with the Oxford/AstraZeneca jab.
Read the latest coronavirus news:
- Oxford/AstraZeneca vaccine turns cells into ‘little factories’ to fight off COVID-19
- Vaccination alone is not enough to contain COVID-19
- What do we know about the delay in the UK’s vaccine supply?
How rare are these blood clots?
Very very very rare. As far as recent studies into the vaccine show, there is a risk of about four in one million of developing a blood clot – and one in a million of dying. This is the estimated risk of dying on a 400km car journey.
Other medications offer a much higher chance of producing a blood clot. While there is a 1 in 250,000 chance of developing a blood clot after being administered with the Oxford/AstraZeneca vaccine, there is a 1 in 2,000 risk of such a clot if taking oral contraception regularly.
Furthermore, your chances of developing a blood clot after being infected with coronavirus are much higher. As Professor Sir Munir Pirmohamed, the chair of the Committee of Human Medicines, recently outlined in a briefing, clotting on the lungs (pulmonary embolism) occurs in 7.8 per cent of people who have COVID-19. Additionally, COVID-19 causes strokes in 1.6 per cent of people.
“All this means is every day you delay getting the AstraZeneca vaccine when it's offered to you, it's a day in which you could be exposed to the virus,” saysDr David Matthews, virologist from the University of Bristol.
“Even if you are young and not likely to suffer the ultimate price from infection, you could still get long COVID, which affects all ages.
“Just think that every medicine comes with these tiny risks. Just open any packet of any medicine you can find in your house and read the patient information leaflet. It’ll all be there at the bottom.”
Are younger people more likely to get blood clots from the Oxford/AstraZeneca vaccine?
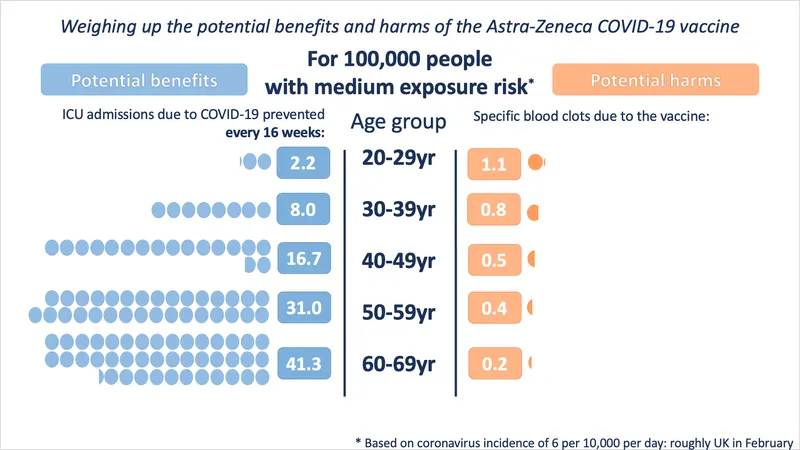
Although younger people are being offered an alternative vaccine to the Oxford/AstraZeneca jab, this does not mean they are significantly more likely to develop blood clots from the vaccine.
Instead, under 30s are being offered a different jab as their chances of dying from coronavirus are very small – so small it’s somewhat comparable to their tiny risk of suffering serious side effects from the Oxford/AstraZeneca vaccine.
Or to put it another way, everyone over 30 should take whatever vaccine they’re offered because the risks of waiting longer to get a coronavirus vaccine hugely out weight the potential, not fully understood, risk of taking the vaccine.
“Yes, you could probably say to under 30s that, just in regards to blood clots, some other vaccines may be healthier or safer for you. But that’s just from the information you have today. This might change. At the moment it’s such low numbers, we can’t really tell,” adds Bamford.
Is the Oxford/AstraZeneca jab less safe than other vaccines?
It’s easy to assume that due to the risk of blood clotting, however small, the Oxford vaccine is not as safe as other vaccines. However, as Matthews explains, it may simply be too early to tell which vaccine is the safest.
“It's going to be a long time before the post-match analysis where we work out exactly what the precise risks and benefits were to every conceivable group of people with every conceivable pre-existing medical condition were,” he says.
“A certain vaccine may conceivably have one advantage or disadvantage that we just don’t know about yet."
Indeed, recent data has changed views on initial vaccine efficacy rates.
For example, initial trial data suggested that the Pfizer vaccine was more than94 per cent effective in over 65s, while the Oxford/AstraZeneca was 70 per cent effective in preventing people from being infected with coronavirus. However, real-world studies have suggested that the Oxford/AstraZeneca is more slightly effective at preventing over 80s being admitted to hospital (80.4 per cent), compared to the Pfizer vaccine (79.3 per cent).
“Future data could show something different for different demographics – it’s very tricky to choose one vaccine over the other. We should focus on the idea that all the vaccines are great. Just get one in your arm!” says Matthews.