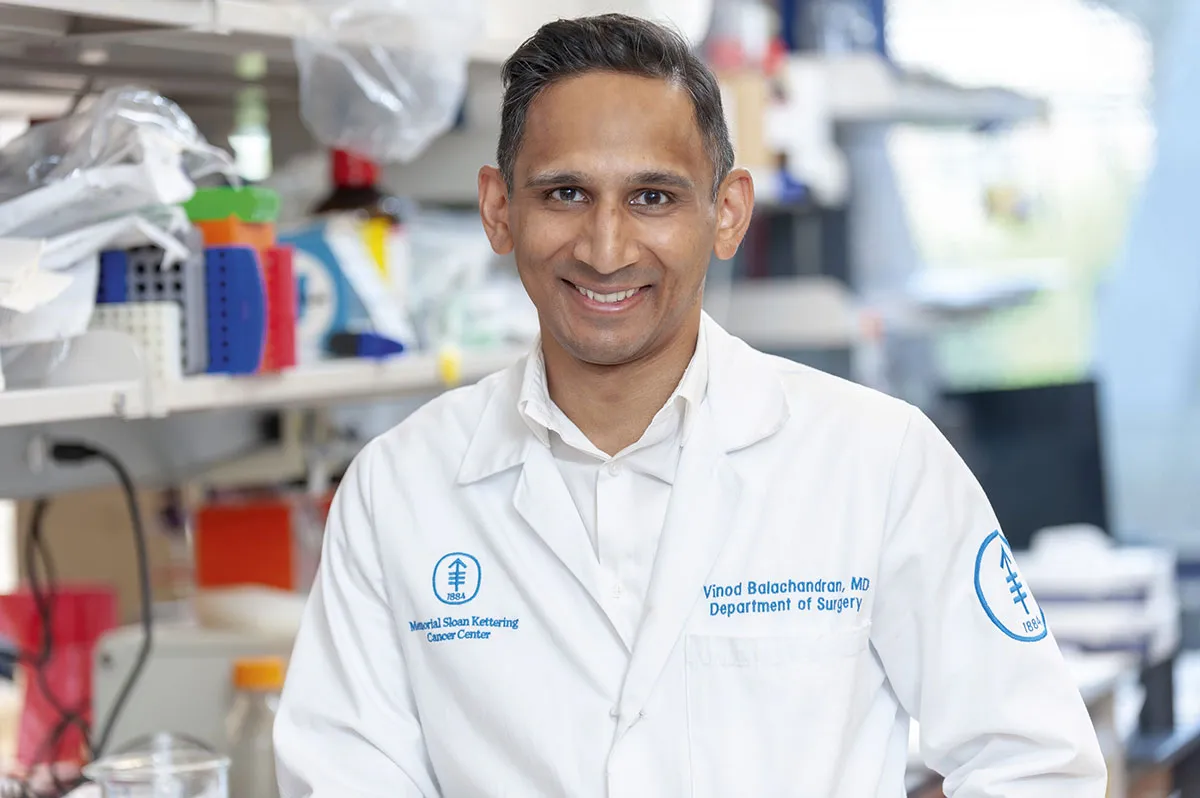
In December 2019, Dr Vinod Balachandran and his team had just recruited the first patients for an exciting clinical trial that was happening in New York. It was to test a new type of vaccine for pancreatic cancer.
The vaccine, made from a molecule called messenger ribonucleic acid (mRNA), was designed to prime the patients’ immune systems to attack their cancer cells, but before the trial could get into full swing, disaster struck. A novel virus, discovered in China, was silently spreading around the globe. Three months later, New York was in lockdown.
With a lot of routine cancer treatment paused, trial participants were understandably nervous. “Patients didn’t want to travel to New York,” says Balachandran, who is based in the city’s Memorial Sloan Kettering Cancer Center.
Then there were logistical issues. Biopsy samples taken from the participants had to be sent to a biotech company in Germany for analysis, and the vaccine, which was then tailor-made for each patient, had to be promptly sent back. With many routine flights grounded, it seemed like a tall order, but perhaps the biggest hurdle facing the trial was the fact that the German biotech company they were working with, BioNTech, now found itself embroiled in a race to produce the world’s first vaccine for COVID-19.
In the year that followed, BioNTech collaborated with another company, Pfizer, to produce more than 20 candidate COVID-19 vaccines, all made from mRNA, including the one that went on to be given to hundreds of millions of people. It’s fair to say that 2020 was a busy year for BioNTech, so you’d be forgiven for presuming that the trial for the cancer vaccines fell by the wayside, but that wasn’t the case.
“Instead of slowing the trial down, we actually accelerated it,” says Balachandran. Balachandran managed the patients, BioNTech made the cancer vaccines, and a trial that was originally scheduled to take two and a half years was completed in 18 months.
Counterintuitively, the diversion that threatened to derail BioNTech’s involvement in the cancer trial – the rapid production and roll out of an mRNA vaccine for COVID-19 – may actually have been a blessing.
Before the pandemic, few people had heard of mRNA vaccines. Investors were disinterested and many scientists were sceptical because mRNA is a notoriously unstable molecule. To top it all, no vaccine of this type had ever been authorised for use. It took a global pandemic and the release of not one, but two mRNA vaccines (from Pfizer/BioNTech and later, Moderna), to prove that these vaccines are safe and that they work.
As a result, mRNA vaccines are generating quite a buzz. They’re exciting because they have the potential not just to prevent disease, but in some cases, to treat it. And because they can train the immune system to recognise problem proteins and cells, as well as problem viruses and bacteria, they have the potential to target not only infectious diseases, such as COVID-19 and malaria, but also some non-infectious diseases, such as cancer and multiple sclerosis.
How do mRNA vaccines work?
mRNA vaccines are fundamentally different to conventional vaccines. Most regular vaccines work by delivering either a dead or inactivated version of a pathogen, or a protein from that pathogen, into the body. Immune cells in the body recognise key proteins in the vaccine, known as antigens, priming the immune system to respond quickly if it later encounters the pathogen for real.
Vaccines like this can take months to make because the viruses have to be grown inside chicken eggs or mammalian cells. Then, when new strains or variants crop up, the vaccine-making process has to start over.
In contrast, mRNA vaccines are made from a type of genetic code. The code exists as a molecule that occurs naturally in the body, where it directs the production of proteins, and when lab-made mRNA is injected into the body, it does exactly the same thing. Specific proteins are produced, and an immune response can be triggered.
The mRNA inside the Pfizer/BioNTech COVID-19 vaccine, for example, directs the body to produce the spike protein that surrounds the coronavirus. There’s no need for chicken eggs or cell cultures, because the process relies on the body to assemble the antigens.
“The body is the best manufacturing facility that we have,” says Dr Lucy Foley, the director of biologics and COVID response at the Centre for Process Innovation in Darlington, in the north of England. Experimental vaccines can be generated in just one week and because the sequence of the RNA molecule can be easily tweaked, existing vaccines can be altered with ease. This is useful, for example, when new variants of a pathogen evolve. “It’s a great platform technology,” she says.
In themselves, cancer vaccines are nothing new. Since it was first introduced in England in 2008, the human papillomavirus (HPV) vaccine has led to an 87 per cent reduction in cervical cancer. Similarly, immunisation with a vaccine against the hepatitis B virus (HBV) can help to protect people against liver cancer.

Both of these non-mRNA vaccines work by targeting cancer-causing viruses, but most cancers aren’t caused by viruses. This is where mRNA vaccines for cancer can make a difference. By training someone’s immune system to recognise tumour antigens, rather than viral ones, mRNA vaccines offer the potential to target a much broader range of cancers.
The problem, however, is that cancer cells are notoriously good at hiding from the immune system, which makes designing the vaccines tricky. In addition, cancer comes in many guises. Breast cancer is different to lung cancer, which is different to melanoma, and no two breast cancers or lung cancers or melanomas are the same.
Put simply, everyone’s cancer is unique. “Every patient’s cancer contains mutations that are particular to them,” says Balachandran, so one approach is to make vaccines that are personalised to each patient.
It’s a far cry from the mass-produced ‘off the shelf’ vaccines that are used against COVID-19 and seasonal flu. After complex surgery to remove their patients’ pancreatic tumours, the team in New York sends samples of the cancerous tissue and healthy blood to the BioNTech laboratories in Mainz, Germany.
The DNA inside these samples is then deciphered, or ‘sequenced’, and the genetic codes are compared. Key differences are identified between the diseased and healthy tissue, and an algorithm is used to predict which of these differences will translate to produce the strongest immune response. “Essentially, we’re asking, how different are the mutations in the cancer cells from the healthy tissue?” says Balachandran.
The top 20 candidates are identified, and their corresponding mRNA sequences are then used to form the basis of the vaccine. By including 20 different mRNA sequences in the mix, the vaccine is designed to teach the recipient’s immune system to recognise not one, but 20 different antigens, boosting the chances that the vaccine will be successful.
Meanwhile, as the vaccine is being assembled in Germany, the patient in New York receives a dose of a drug called a checkpoint inhibitor, which is used to boost their body’simmune response to cancer cells. Then, nine weeks after undergoing surgery to remove the tumour, the vaccine arrives in the Big Apple, and each patient receives their own bespoke version, delivered deftly into their arm.
Read more about cancer vaccines:
- Revolutionary cancer vaccine trials inspired by COVID jab begin
- Personalised cancer vaccine 'activates immune system' in early trials
Early trial results
Balachandran’s is one of a growing number of early phase clinical trials seeking to assess the safety and tolerability of mRNA vaccines for a wide range of cancers, including those affecting the ovaries, brain and lungs. Glimmers of hope can be seen. A 2017 study of a personalised mRNA vaccine for advanced melanoma, for example, showed that it reduced the risk of the cancer spreading.
“It’s too soon to talk about efficacy in our trial,” says Balachandran, “but I’m optimistic.” Pancreatic cancer has the lowest survival rate of all common cancers. Around 90 per cent of people who have it die within five years of diagnosis, because their cancer keeps coming back. By priming the immune system to destroy any cancerous cells that do occur, the hope is that both remission and life will be longer.
Elsewhere, other mRNA vaccines are seeking to exploit the similarities that exist between different people’s cancers, rather than the differences. People with a type of breast cancer known as HER2-positive, for example, are often treated with an antibody-based drug called Herceptin. The treatment can work well initially, but then the cancer cells evolve resistance to it and the drug stops working.
It’s similar to the way that bacteria develop resistance to antibiotics, only here the cancer cells evolve in a very predictable manner. Specific mutations crop up in specific genes.
Dr Herbert Kim Lyerly from Duke University has designed an mRNA vaccine that targets four of these known mutations, and in 2022 it will be tested in a small number of patients with advanced HER2-positive breast cancer. Every patient will receive the same vaccine because every one of them is expected to develop the same key mutations. “We’ll effectively be vaccinating people against mutations that their cancer doesn’t yet have,” explains Lyerly.
Then, when cancer cells with the mutations do appear, as is highly likely, the patients’ immune systems should be ready to hunt them down and destroy them. If it works, the vaccine will prevent their cancer from evolving resistance to Herceptin, so a drug that works well initially can continue to work well indefinitely. “The hope would be that you would never run out of treatment options,” says Lyerly.
This isn’t just ‘treating’ cancer, it’s anticipating and then preventing cancer. As more becomes known about the genetic progression of different cancers, it’s entirely conceivable that the same approach could be applied to other cancers too.
Suppose someone has a family history of a particular cancer, or genetic tests reveal that they have a heightened risk. If the genetic hallmarks of that cancer are predictable and well known, and if the technology is available, then an mRNA vaccine could be used to prime their immune system to destroy the cancer at source. “My gut feeling is that the technology is moving in this direction,” says Dr Samuel Godfrey, the senior science communications manager at Cancer Research UK.
There are caveats of course. Many promising early-stage treatments flounder the more they’re tested, and Godfrey points out that a vaccine or treatment that works for one person may inexplicably fail for another. Nor is the Holy Grail of cancer therapy – a single shot to prevent all cancers – likely to happen. Cancer is a diverse collection of diseases that is far too complex to be beaten by a single approach. More likely, then, is that if mRNA vaccines prove their worth in clinical trials, they’ll go on to be used alongside other therapies, such as antibodies, surgery and chemotherapy.
Nevertheless, the promise of mRNA vaccines, not just to treat certain cancers, but also to prevent them, remains firmly on the cards. “We’re getting to a point where we can start to be proactive with cancer as well as reactive to it,” says Godfrey. “I think it’s phenomenally exciting.”
Where else could mRNA vaccines work?
Malaria
In 2021, the World Health Organization approved the first mass rollout of a vaccine for malaria, but it’s far from perfect. Although it is not an mRNA vaccine, it reduces disease severity and prevents cases in around 40 per cent of people.
A key problem with making a malaria vaccine is that the parasite responsible for the disease has evolved a way to prevent the immune system from remembering it. Richard Bucala, professor of medicine, pathology, and epidemiology and public health at the Yale School of Medicine, has shown the involvement of a key parasite protein, called PMIF, which suppresses the host’s immune system and prevents it from making key immune cells.
Working with the drug company Novartis, Bucala has developed an mRNA vaccine that targets this protein, and which has been shown to help protect mice against malaria infection. Now Bucala has joined forces with scientists at Oxford’s Jenner Vaccine Institute, and they hope to test the vaccine in people later in 2022.
Multiple Sclerosis

Multiple sclerosis (MS) occurs when the body’s immune system malfunctions and starts destroying the fatty myelin coating that surrounds nerve cells. With assistance from BioNTech, German researchers have devised an mRNA vaccine that encourages the immune system to tolerate the myelin protein, rather than attack it.
Research published in 2021 showed that the vaccine delayed the onset and lessened the severity of an MS-like disease in mice. It’s an encouraging result. Current MS treatments work by targeting the immune system as a whole, which means the drugs often cause side effects. The mRNA vaccine, in contrast, is designed to target only those cells that attack the myelin, so side effects could be minimised.
It’s early days, though, and there are, as yet, no clinical trials for MS mRNA vaccines in patients.
HIV
It’s not easy to make an HIV vaccine because the virus mutates quickly, so it’s hard to find a stable target for a vaccine. But Dr Derek Cain from Duke University has shown that some patients with chronic HIV develop antibodies that can neutralise the virus.
Unfortunately, the antibodies do little to help the patients because there’s already too much virus in their bodies, but if an HIV-free person could produce the same antibodies, it might help protect them from future infection.
Last year, a vaccine based on this idea was tested in a small human trial. In total, 97 per cent of those who received the vaccine produced the immune cells needed to generate the antibodies. “This study demonstrates proof of principle for a new vaccine concept for HIV,” says Dr William Schief, who worked on developing the vaccine.
- This article first appeared inissue 372ofBBC Science Focus Magazine–find out how to subscribe here
Read more about the future of cancer treatment:

