An NHS hospital which upgraded the type of face masks used by staff on COVID-19 wards saw a dramatic fall in hospital-acquired coronavirus infections among those workers, by up to 100 per cent, research has indicated.
Addenbrooke’s Hospital in Cambridge upgraded the masks used by staff on COVID-19 wards from fluid-resistant surgical masks (FRSMs) to filtering face piece 3 (FFP3) respirators, with the change made in late December 2020 in response to its own staff testing data.
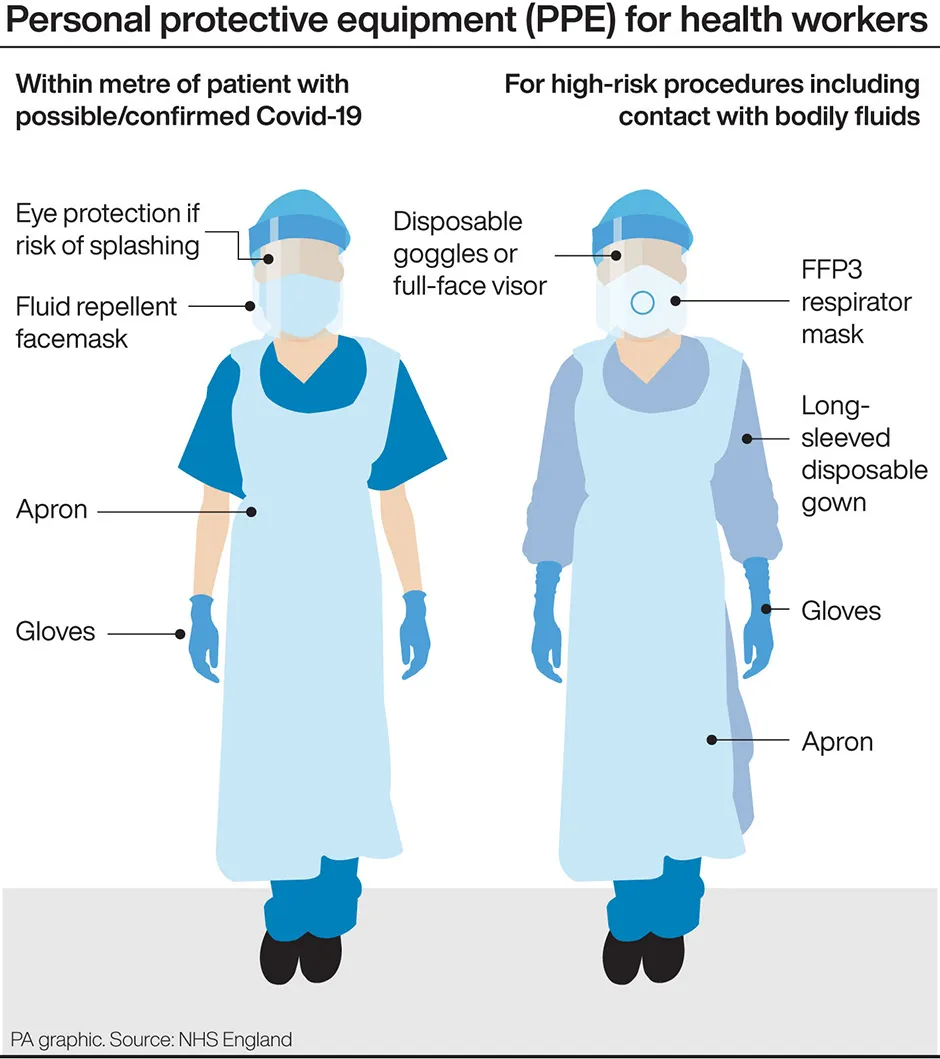
The UK Infection Prevention Control (IPC) cell had, until recently, recommended that healthcare workers caring for COVID-19 patients should use FRSMs as respiratory protective equipment. The IPC cell recommended that an FFP3 respirator should be used if an aerosol-generating procedure were being carried out, such as inserting a breathing tube into the patient’s windpipe.
Guidance has recently been updated to oblige NHS organisations to assess the risk that COVID-19 poses to staff and provide FFP3 respirators where appropriate.
Addenbrooke’s has been testing staff for COVID-19 since the start of the pandemic, even when workers showed no symptoms. This testing programme indicated that healthcare workers caring for COVID-19 patients were at greater risk of infection than staff on non-COVID-19 wards, even when using the recommended respiratory protective equipment.
In response, the hospital’s infection control committee upgraded the type of masks used by staff on COVID-19 wards.
Read more about face masks:
- Should I wear two masks to prevent the spread of COVID-19?
- Why is it more annoying seeing someone wearing a face mask incorrectly than seeing someone not wearing a mask at all?
- Face masks: Are they changing how we behave?
Prior to the upgrade, COVID-19 cases were higher among staff on COVID-19 wards compared with non-COVID-19 wards in seven out of the eight weeks analysed by researchers. Following the change in protective equipment, the incidence of infection on the two types of ward was similar.
The research has not yet been peer-reviewed, but is being released early because of the urgent need to share information relating to the pandemic.
“Before the face masks were upgraded, the majority of infections among healthcare workers on the COVID-19 wards were likely due to direct exposure to patients with COVID-19," said Dr Chris Illingworth, from the MRC Biostatistics Unit at Cambridge University.
“Once FFP3 respirators were introduced, the number of cases attributed to exposure on COVID-19 wards dropped dramatically – in fact, our model suggests that FFP3 respirators may have cut ward-based infection to zero.”
According to the researchers’ mathematical model, the risk of direct infection from working on a non-COVID-19 ward was low throughout the study period, and consistently lower than the risk of community-based exposure.
By contrast, the risk of direct infection from working on a COVID-19 ward before the change in respiratory protective equipment was considerably higher than the risk of community-based exposure: staff on COVID-19 wards were at 47 times greater risk of acquiring infection while on the ward than staff working on a non-COVID-19 ward.
“Our data suggests there’s an urgent need to look at the PPE offered to healthcare workers on the frontline," said Dr Michael Weekes, from Cambridge University’s Department of Medicine.
“Upgrading the equipment so that FFP3 masks are offered to all healthcare workers caring for patients with COVID-19 could reduce the number of infections, keep more hospital staff safe and remove some of the burden on already stretched healthcare services caused by absence of key staff due to illness.
“Vaccination is clearly also an absolute priority for anyone who hasn’t yet taken up their offer.”

A Department of Health and Social Care spokesperson said: “The safety of the NHS and social care staff has always been our top priority and we continue to work round the clock to deliver PPE to protect those on the front line.
“Guidance on the appropriate levels and standards of PPE is written by experts and agreed by all four UK chief medical officers.
“Updated infection prevention control guidance was published this month [June] to reflect the latest scientific understanding on how to prevent transmission of COVID-19.
“Emerging evidence and data are continually monitored and reviewed and guidance will be amended accordingly if appropriate.”
Read more about COVID-19: