It seems the more we learn about COVID-19, the more menacing it becomes. Why does COVID-19 affect people so differently? Are some of us already immune? And how do the potential vaccines work?
As scientists race towards a vaccine, we report on the latest discoveries helping us understand how our immune system handles the infection.
Why does COVID-19 affect people so differently?
The wide range of outcomes of being infected with COVID-19 – from showing no symptoms at all, to rashes, severe respiratory illness and death – reflects the huge variation found in people’s immune systems. How the immune system responds to a virus such as SARS-CoV-2 is influenced by many factors, from our genes and general health to the other pathogens we’ve encountered in the past.
With COVID-19, there seems to be a critical period during which the immune system either mounts a protective response, stifling the virus and slowing its spread in the body, or a dysfunctional, inflammatory response, where the body starts to attack itself.
As part of a healthy immune reaction, local white blood cells recognise the virus as foreign and release chemicals called cytokines. These molecules help direct and amplify the body’s immune response, which can limit the spread of the virus and kill off infected cells. But the release of too many cytokines in a short period can start to cause collateral damage to healthy cells.
In critical cases of COVID-19, the acute lung problems that are characteristic of the disease are caused by a ‘cytokine storm’ – a dangerous runaway overreaction of the immune system that creates even more inflammation and tissue damage than the virus.
Read more about COVID-19:
“We know that as we age, our immune systems are not as good at clearing infections,” says Dr Elizabeth Mann, an immunologist who has been following the progress of COVID-19 patients arriving at hospitals across Manchester. “Older people are also predisposed towards the types of inflammatory immune responses that cause damage in COVID-19.”
As well as age, genetics also have a role to play. A recent case study that looked at four young males with severe COVID-19 found that all four had rare genetic alterations in a particular gene that helps modulate the immune response.
Worryingly, in those instances when COVID-19 does cause severe illness, the effects on the regulation of the immune system can be long lasting, according to Mann.
“We’re also seeing long-term abnormalities in some immune cells in the blood that persist for several months following discharge,” says Mann. “This indicates that the immune system doesn’t simply reset and go back to normal upon recovery.”
It goes without saying that people taking certain medications that suppress their immune systems – such as those who have HIV or have recently had an organ transplant – are at risk of having a weakened or dysfunctional immune response.
We also know that certain ethnic groups, such as black and Asian people, are more likely to die from COVID-19. Studies are looking at why the mortality risk is greater for people in these ethnic groups, and differential immune system reactions could be part of a spectrum of factors alongside economic, cultural and health reasons.
There is also some evidence that the ‘dose’ of virus you receive can be a factor in how your immune system copes with the infection. For example, a ‘low dose’ might involve picking up a few viral particles from a surface and then scratching your nose. But sharing a small space with an infected person who is coughing and spluttering would mean breathing in lots of viral particles, resulting in a much larger amount of viral particles entering the lungs all at once.
Does having COVID-19 antibodies mean you’re immune? And is everybody whohas recovered fromCOVID-19 immune?
Once the immune system has started to fight a virus, it creates specific antibodies for that particular pathogen. These Y-shaped proteins circulate in the body and stick to anything resembling the virus, acting like a flag that tells other immune system cells to destroy it.
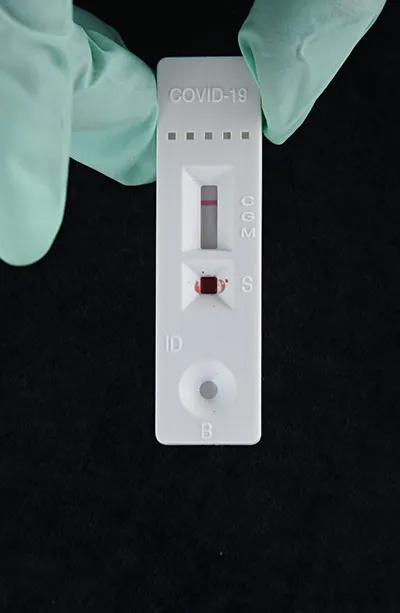
The presence of antibodies specific to COVID-19 in the blood has therefore been used to test if somebody has had COVID-19 and is ‘immune’ from getting it again. Governments around the world have considered issuing people with ‘immunity certificates’ or immunity passports, including the UK, which suggested people might be given special bracelets if tests show they have COVID-19 antibodies.
Unfortunately, the messy reality of the immune system mean it isn’t that simple. Firstly, a certain percentage of the population, perhaps as many as 20 per cent, just don’t seem to make antibodies to COVID-19, making it harder to tell who has and hasn’t had it. Even when people do make antibodies, the number of those antibodies circulating in the blood can fade rapidly once that person has recovered, to the point where it may be impossible to detect any antibodies at all after a few months.
Read more
- COVID-19 'highly likely' to become seasonal disease
- Scientists think they’ve identified how COVID-19 causes patients to lose their sense of smell
While this may seem like bad news, fluctuations in antibody levels are a normal part of immunity, says Dr Kaitlyn Sadtler, an immunologist from the USA’s National Institutes of Health.
“There are viral infections that induce lifelong antibody responses, but antibody responses to respiratory viral infections often do wane. Vaccination [and immunity] is not a binary – it’s not that it 100 per cent works or it 100 per cent doesn’t work. For certain viruses, we need an initial dose and then a further one or two boosts – others might require seasonal vaccination or vaccination every few years.”
Antibodies aren’t the only way the body remembers a virus, either. “Antibody tests are quick and inexpensive, but there are also other parts of the immune system beyond antibodies that help with our immunity,” says Sadtler.
Components of the immune system known as T-cells help identify cells in the body that have been infected with the virus and also help guide the production of antibodies. Even if a person has no detectable antibodies left, the T-cells will be primed to ensure the immune system responds to the threat more quickly than the first time.
Do some people in thepopulation alreadyhave some resistance to COVID-19?
Possibly. Studies have shown that some people who haven’t had COVID-19 show some innate immune ‘reactivity’ to proteins found in SARS-CoV-2. These people didn’t have COVID-19 antibodies, but their T-cells seemed primed to respond to the virus, at least in laboratory tests.
Scientists hypothesise that this could be a result of exposure to other coronaviruses, such as the common cold or the SARS virus, which circulated in 2003. Some studies suggest up to 50 per cent of people might have this underlying ‘reactivity’ to coronaviruses (to call it ‘resistance’ is probably overstating the effect), which could help them get away with milder symptoms.
Interestingly, it’s believed that the common cold was once a far deadlier coronavirus, like SARS-CoV-2 is now. Having circulated for thousands of years, humans have developed a broad immune response that ensures infection with a new strain of the cold virus results in only mild symptoms.
Some scientists believe that without a vaccine, COVID-19 will eventually go the same way, circulating for many years until almost everybody has some kind of broad immune system memory to it that helps fight off newer or more severe strains.
How do potential COVID-19 vaccines work?
There are currently over 150 vaccines in trials around the world. Like any immunisation, the COVID-19 vaccines in development aim to help us develop immunity to the virus without having to go through the danger of a real infection.
The ‘traditional’ way to do this would be to present the body with a damaged or inert version of the virus, allowing the immune system to learn how to fight it without the possibility of the virus doing any harm or replicating in the body.
As well as traditional vaccines involving a weakened or inactive version of the SARS-CoV-2 virus, a range of more modern approaches are being trialled. Some vaccines are made up of just a small part or subunit of the virus, such as the spike protein that SARS-CoV-2 uses to attach to our cells. This spike protein is completely unique to the SARS-CoV-2 virus, and so if the immune system develops a robust immune response to the protein, it should also react strongly to the real virus, which is coated in it.
Another approach is to use what are known as ‘genetic’ vaccines. These vaccines contain a specific sequence of DNA (or its chemical cousin, RNA) from the virus. Once this bit of genetic code is injected into the body, the body’s own cells then synthesise that bit of the virus, which the body recognises as foreign, causing it to induce an immune response.
Other components can be added to such vaccines to encourage the immune system to respond, for example, special molecules that create a strong immune response known as adjuvants, or by incorporating the genetic vaccine into a different, harmless virus.
All the different types of vaccine have pros and cons. “For success in this pandemic, our best bet is to ensure we have multiple horses in the race,” says Prof Trevor Drew, director of the Australian Centre for Disease Preparedness. “Live, attenuated [weakened] vaccines can take a long time to make and there’s the possibility they could mutate to become more dangerous again.
"Subunit vaccines don’t always induce robust immune responses without adjuvants. And genetic vaccines are relatively easy and inexpensive to make, but they’re a new approach and there aren’t actually any existing vaccines of this type [approved for use] yet.”
Any vaccine must pass three strict phases of clinical trial test: checking for safety (phase I), that it works (phase II) and how well it works in large populations (phase III). Despite the best efforts of public health organisations to fast-track these trials and cut down on bureaucracy, just 20 of the potential 150 vaccines currently in development have progressed to human trials so far.
The most advanced candidate so far is being developed by the Oxford University and pharmaceutical giant AstraZeneca. Early results from human trials have been positive and there are plans already taking shape to produce over two billion doses.
The vaccine is made up of a harmless virus that can’t replicate, but contains the gene to produce the SARS-CoV-2 spike protein. In trials involving around 1,000 volunteers, the vaccine provoked a T-cell response within 14 days of vaccination and an antibody response within 28 days.

“We’re using replication-deficient adenoviruses because they can’t spread and they’re very safe,” says Prof Sarah Gilbert, one of the Oxford University vaccinologists working on the vaccine.
“They’re also very good at inducing an immune response to the gene that you’ve added to them, because you’re actually getting a viral infection. So when you vaccinate somebody, the adenovirus goes into cells at the injection site – it infects them. The cells react as if there’s an infection and the antigen that’s been produced in large quantities is the coronavirus spike protein.
“The immune cells in the body haven’t seen that spike protein before. So that’s what they latch on to and you get a strong immune response to it. As the adenovirus can’t replicate, it’s lost from the body pretty quickly, so you’re left with that immune response and the memory immune response.”
There are still many steps required to prove that the vaccine’s effects actually prevent COVID-19 infections and that the effects last; more tests are needed to ensure it’s effective and safe to use in more vulnerable groups, such as older people or pregnant women. Gilbert has been inundated with people asking when the vaccine will be ready and the truth is, it’s impossible to say.
“We have to have three things: we have to prove vaccine efficacy, there has to be large amounts of vaccine made, and we need regulatory approval. We can’t tell the timing on any of them very precisely.”
Before a vaccine isavailable, is thereanything people cando to make sure their immune system is ingood shape?
Researchers have been studying the effects of diet, exercise, psychological stress and other factors on the immune response to COVID-19. There’s good data to suggest that your general health does make a difference to how your immune system copes with COVID-19.
Having high blood pressure or heart disease, or smoking, can increase the likelihood that you’ll be hospitalised from COVID-19. Public Health England released a report on how being obese or excessively overweight increases the risk of illness and death from COVID-19 and there’s some evidence of a link between vitamin D deficiency and COVID-19 severity.
“Maintaining a healthy lifestyle with regular exercise, a balanced diet, adequate sleep and minimal stress has been shown to keep our immune system strong and healthy,” says Dr Madhvi Menon, a research fellow working at Manchester University’s Institute of Immunology and Infection. “But very little is currently known about ways to avoid the severest form of COVID-19.”

It’s just as important to be sceptical about anything that claims to be able to ‘boost the immune system’ or ward off COVID-19. During the Spanish flu in 1918, which killed an estimated 50 million people, everything from onions to masturbation were touted as ways to boost the body’s defences against the virus, and the pandemic of 2020 has been no different.
Social media is awash with misinformation claiming anything from eating garlic to drinking silver can boost the immune system. Donald Trump, the US president, has added to the confusion by promoting the drug hydroxychloroquine as a preventative of COVID-19, when there is no good evidence that it is.
The best thing you can do to protect yourself is to not get COVID-19 in the first place. By adhering to guidance on social distancing, masks and frequent hand-washing, you’re not only protecting yourself, but you’re also helping prevent the disease spreading and saving vital health system resources for those who need it most.
- This article first appeared in issue 354 of BBC Science Focus Magazine–find out how to subscribe here
