Materials scientist Gordon Wallace is the director of ARC Centre of Excellence for Electromaterials Science at the University of Wollongong, New South Wales, Australia. He is developing the ‘sutrode’, a medical device made from graphene that combines the electrical properties of an electrode with the mechanical properties of a suture.
The device is wrapped around damaged or malfunctioning nerve bundles and used to stimulate them and return their regular function. Though still in its early stages, the technology may one day be used to treat epilepsy, schizophrenia, and in the production of next generation prosthetics.
He speaks to BBC Science Focus commissioning editor Jason Goodyer in this episode of theScience Focus Podcast.
We now have more than 75 episodes of theScience Focus Podcast, each of which is still well worth a listen. Here are a few that you might find interesting:
- Is the cure for cancer hiding in human breast milk? – Professor Catharina Svanborg
- Is gene editing inspiring or terrifying? – Nessa Carey
- Can we slow down the ageing process? – Sue Armstrong
- What is your brain doing while you sleep? – Dr Guy Leschziner
- What does a world with an ageing population look like? – Sarah Harper
- Is racism creeping into science? – Angela Saini
Read the edited interview fromBBC Science Focus Magazine
What are ‘electroceuticals’?
The name’s derived as an alternative to ‘pharmaceuticals’. So, ‘electroceuticals’ is the use of electrical stimulation to treat specific diseases by targeting particular nerves, guiding particular organs. The challenge to date has been to find tools that can communicate with our nervous system with enough resolution or accuracy to target specific nerves.
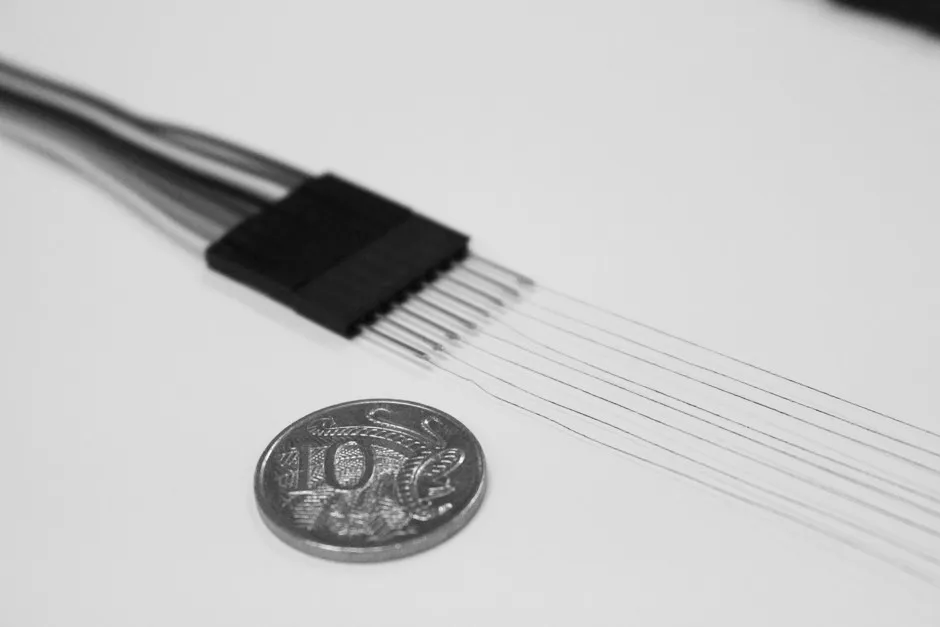
You are making ‘sutrodes’. What are they made from?
They’re threads made of graphene. This wonder material keeps turning up in all sorts of areas. Graphene’s just a single sheet of carbon that was discovered not many years ago, for which the Nobel Prize was attributed. There has been an explosion of interest in the material, and the very simple and elegant chemistries that allow us to take a lump of graphite – the kind that you’d find in a lead pencil – and exfoliate or explode it into single sheets of graphene.
We do that in such a way that we can control the size of the sheets and also control the amount of oxygen that is on the sheets. That gives us this combination of electrical properties and processability – the ability to make the fibres. A cocktail of clever chemistries that delivers both of those properties has enabled us to make this particular advance.
How does it work?
By working with our collaborator Prof Mario Romero-Ortega at the University of Texas, Dallas, we have demonstrated that we can actually tie these electrodes around small nerve bundles going into organs – the spleen in this case. That’s why we call it the sutrode, because it has the basic mechanical properties of a suture, and yet all of the properties of an electrode. Importantly, it’s an electrode that’s compatible with a living, pulsating system.
What results have you had?
Mario and I have both been interested in the field of electroceuticals for some time. In particular, whether the electrical stimulation of the nerves going under the spleen can regulate the immune response. Now, with these new tools, he’s shown that we can definitely record signals from the nerves going into the spleen and that there are different levels of communication through each of those different nerves.
The studies are looking at whether you really can regulate the immune response through electrical stimulation of those different nerve types. Before this, you would have to track back to bigger nerve bundles to use conventional electrodes and so you didn’t have that specificity of communication – whether that’s for recording or stimulation – that we have now.
What sort of conditions or diseases could this help treat?
At the moment, our studies are focused on the use for nerve and muscle regeneration. In the regeneration studies, and in the electroceutical area, the focus with Mario is on further studies into how we can regulate the behaviour of the spleen through electrical stimulation. And as I say, that regulates the immune response.
But we envisage that as others become aware of what the sutrodes can do, they will establish, or try to establish, collaborations with partners around the world to target other specific diseases using their biological or medical insights into those diseases and our ability to produce the devices and structures.
So it treats a disease by doing what a healthy, functioning nervous system would be doing?
Yes, so in terms of the electroceuticals, it’s trying to restore the natural behaviour of the neurosystem [nervous system] in controlling organs.
In terms of nerve or muscle regeneration, the sutrode promotes the healing process by providing a conduit that facilitates the repair or regrowth of nerve connections, or the alignment and restoration of muscles.
Read more about the future of medicine:
What is going on in this nerve bundle when it gets stimulated by the sutrode?
We’re just learning about that. We’ve been able to show that we can record, with incredible sensitivity, the electrical impulses that are generated by this nerve bundle. And then we’re figuring out what those different electrical impulses do to the organ, and what biological responses can be regulated. By superimposing electrical impulses from our sutrode over this system, we hope we’ll be able to influence how it works.
What advantages would this sort of treatment have over regular medicines, like injections and tablets?
I think the ability to target the disease more specifically. The ability to deliver the stimulation when it’s needed to treat those diseases, and in some cases, potentially, a much more effective way of actually treating particular diseases.

Diseases like epilepsy or schizophrenia are not very well treated by normal pharmaceutical approaches, and treatment often ends up being a cocktail of drugs that are personalised for that individual. It’s basically a trial and error process.
Will the sutrodes be put into the affected area and then left there? Or are they for short-term use?
Look, in terms of electroceuticals, the real answer to that is we don’t know. Can you actually reverse the disease by electrical stimulation for a certain period, and then not need to stimulate any further? These are all studies that need to be done.
In terms of other applications of these sutrodes, for example, in nerve repair, nerve regeneration or muscle regeneration, because of the mechanical properties of the fibre, we envisage it will be fine just to leave them in there to do the repair and then to leave them as part of the naturally restored system.
Read more about future technology:
In terms of cost, how do these compare to traditional medicines?
The cost of the actual materials is incredibly low. We’re talking about graphite out of a mine, and simple chemistries and fabrication methods to make them. So, there’s no huge cost involved in that. And in terms of the hardware to drive them, the cost is low as well. So, materials and fabrication costs are quite low compared to if you were developing a whole manufacturing process for a new pharmaceutical, for example.
What will the future of this research look like?
The focus in the near future will be in nerve and muscle regeneration. We will, of course, pursue different areas of electroceuticals with collaborators as we establish them. One other area that will use these materials, given their effective ability to communicate with nerves and muscles, is as an interface for neurally driven prosthetics, like a prosthetic hand.
What do you mean by ‘neurally driven’?
Basically, the nervous system will communicate directly and send electronic signals to a prosthetic hand to drive it via a sutrode. And by incorporating sensing technologies into the hand, it will provide sensation back to the user.
So, if I need a prosthetic hand I’d be able to control it in the same way that I control my own hand?
Yes. Exactly. Now, that requires a high-fidelity neural interface to the prosthetic, and we believe that’s exactly what we’ve got in the sutrode, and that’s something we’ll be pursuing.
- This interview was first published in the August 2019 issue of BBC Science Focus–subscribe here.
Follow Science Focus onTwitter,Facebook, Instagramand Flipboard