Scientists are a cautious bunch, fond of a caveat even when describing their own research. “Our favourite expressions are ‘Yes, but…’ and ‘On the other hand...’ and ‘It remains unclear...’” says gene editor Dr Fyodor Urnov. “So please add all of that to what I’m about to say.
"If CRISPR realises 10 per cent of what we practitioners of gene editing dream it to be able to do, it will rival the greatest advances in the history of biomedicine as a technology to impact public health.”
Urnov is talking via a crackly Zoom link from his office at the Innovative Genomics Institute (IGI) in Berkeley, California, which is at the forefront of what may prove to be the defining scientific breakthrough of the 21st Century.
CRISPR is a genome editing technology that allows scientists to cut DNA with incredible precision and insert or delete DNA to correct unwanted mutations. To oversimplify the technology, it’s the power to edit the building blocks of life, just like text on a computer screen. Not only could it enable scientists to switch off genes that lead to a broad spectrum of disease, but it will unshackle all of us from the genetics we’re born with.
“The knowledge gained is amazing and it’s just really accelerated basic research. That in itself is already transformative,” says Dr Robin Lovell-Badge, from the Crick Institute. “And the notion that we can actually treat people with genetic diseases in a way that was never possible before is mind boggling.”
For much of the past decade, the technology has been confined to the lab. Now, though, the first CRISPR therapies are changing the fate of people born with debilitating inherited conditions. Most of us haven’t realised it yet, but we’re in the foothills of a profound medical and technological revolution that raises not only the prospect of new treatments and cures, but also huge questions about ethics, equality and health justice.
The incoming wave of gene-editing applications has been compared to the Industrial Revolution or the birth of the internet in terms of the game-changing impact it will have on society.
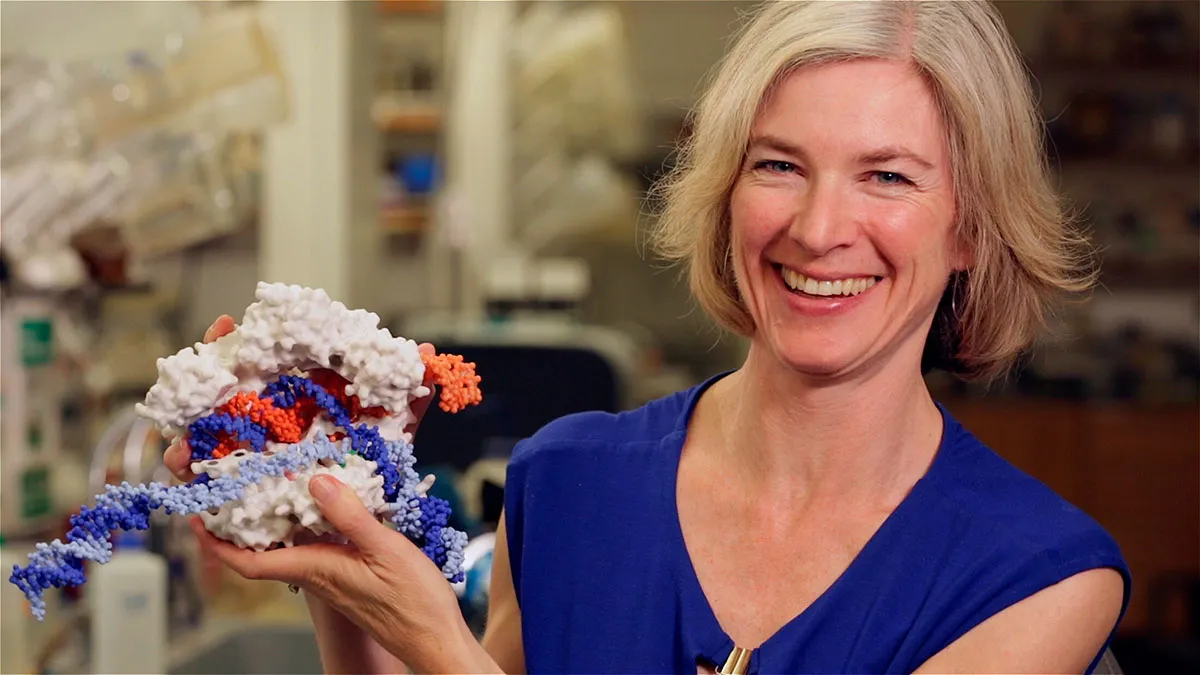
Biochemist Dr Jennifer Doudna established the IGI to tackle all of that and more. As a non-profit organisation, the institute exists not just to research gene editing, but also make it affordable and accessible to everyone. It’s a big claim, given the breadth of CRISPR’s potential, so the IGI’s leadership team agreed to give BBC Science Focus an exclusive overview of its efforts.
It was there on the Berkeley campus where Doudna and Dr Emmanuelle Charpentier changed the world nearly a decade ago. Their collaboration led to the development of CRISPR-Cas9, the gene-editing tool described in a landmark 2012 paper that won a Nobel Prize.
“I think we both had a little sense of, you know, kind of a chill,” she says. “I still remember that feeling of hairs standing up on my neck, thinking there’s something really interesting here. And I would wager that neither of us at the time had any idea where it would end up, because I don’t think one ever does.”
CRISPR isn’t the only gene-editing technology, and the IGI is not the only institute pioneering the field of study. But CRISPR is more versatile, easier to use and cheaper than a lot of other technologies. And what’s astonishing is the speed of progress. In less than a decade it’s gone from discovery to human trials and potential cures, something that’s practically unheard of in biomedicine.
“It’s a little bit of whiplash,” says Dr Brad Ringeisen, executive director of the IGI. “Think about nanoparticles, the nano revolution. Pfizer has nanoparticles in their COVID mRNA vaccine, but that [technology] has taken 30 or 40 years.”
Read more about CRISPR:
- CRISPR gene editing: The key benefits (and risks) of modifying our natural world
- CRISPR scientists awarded 2020 Nobel Prize for chemistry
- Who really discovered CRISPR, Emmanuelle Charpentier and Jennifer Doudna or the Broad Institute?
CRISPR's first successes
People born with sickle cell disease will be among the first to benefit from advances in gene editing. In 2019, a woman called Victoria Gray became one of the first people in the world to be treated for a genetically inherited disease with a CRISPR-based therapy.
Born with sickle cell anaemia, she required strong pain medication and regular blood transfusions to stave off the effects of the mutated gene that makes red blood cells warp and block the flow of blood and oxygen around the body. Aside from bouts of excruciating pain, sickle cell anaemia can lead to stroke, hypertension, organ damage and more.
The treatment was not simple. Doctors removed bone marrow cells from Gray and the other patients in the trial, then used CRISPR to edit a gene that activates production of foetal haemoglobin, a protein that can alleviate the symptoms of sickle cell disease. The patients then underwent chemotherapy to destroy most of their bone marrow, after which billions of edited cells were infused back into their bodies.

Gray no longer requires medication or transfusions, and neither do the other people in her trial, which included patients with a related blood disorder. It seems that a one-time CRISPR treatment has cured them.
“Sickle cell disease is probably the easiest target that affects the most people,” says Ringeisen. “It’s about as simple as you can possibly get: you go in and either turn on an alternative gene or you try to correct the one thing. One hundred thousand people in United States have sickle cell disease and I think it’s over a million people worldwide. So there’s a huge impact that can be had.”
The IGI is preparing its own sickle cell trial, but the institute’s scope also includes many other conditions. As well as blood disorders, it has active research projects on autoimmune disease, neurological disease, cancer and COVID-19. One promising avenue of research is with T-cells, sometimes described as the troops on the ground of our immune system.
Dr Alex Marson, the IGI’s director of human health, is running a lab that is working to engineer T-cells using CRISPR to treat different kinds of disease. He is currently planning a clinical trial with a family where a strong genetic mutation has caused different manifestations of autoimmune disease in the younger generation.
“In the lab we’ve corrected cells from these children,” he says. “Now we’re working towards doing a clinical trial to take those gene-corrected T-cells and infuse them into at least one of these young adults to try to restore balance in the system and treat the autoimmune disease.”
Whereas current T-cell therapies are wildly expensive, Marson envisions a future where off-the-shelf T-cells are manufactured to treat different kinds of disease, their production industrialised to a scale that makes them accessible to anybody who needs them.

“We can treat infectious diseases by designing immune cells that recognise infections,” he says. “I think we’re going to have this sort of flexible ability to actually write the language of the DNA in the immune cell and use it in a drug platform.”
This is where things start getting really interesting, because it showcases just how broad the medical applications of CRISPR will be. Its potential lies not just in those conditions caused by a single genetic mutation like sickle cell disease, but any disease that has a genetic component, either in terms of susceptibility or protection.
That includes many of the major killers, including cancer, cardiovascular disease and neurodegenerative disease, plus chronic conditions like inflammatory bowel disease and rheumatoid arthritis.
“All disease is on the map,” says Ringeisen.
Disease prevention
Part of what gives scientists optimism is that gene editing can be used to bestow protective DNA on a person as well as correcting unwanted mutations.
“We know there is a genetic change you can make that will dramatically lower your risk of heart disease,” says Urnov. “How do we know that? Because of very rare individuals who have those genetic changes. And when you study lots of them, it’s kind of jaw-dropping. I’m not going to say they’re immune to heart disease, but they’re close to it.”
Doudna believes that CRISPR could even be used more to prevent disease than to treat it. “Imagine a time when people get their genome sequenced and be told that you have a gene that makes you have a higher likelihood of getting cardiovascular disease,” she says. “But you have the option of editing your cells so that you don’t have to wait to find out if you’re one of the unlucky folks that is susceptible.”
Today, lots of us take preventative action to protect our future health. It could be anything from eating a high-fibre diet to keep heart disease at bay, to having a double mastectomy because breast cancer runs in the family. Would you be comfortable editing your DNA to achieve the same results?
It’s harder to do the cost-benefit analysis when you’re talking about such experimental therapies. There are some who will say that any form of gene editing is ‘playing God’ and conspiracy theories around COVID-19 vaccines show how mistrust in new technologies can spread.
“There can be misrepresentations or just misconceptions embedded in the public mindset that can have a negative effect on what I think should be positive advances,” Doudna says. “Another example of that is the whole anti-GMO movement.”
In November 2018, twin girls were born in China, the so-called CRISPR babies. Biophysicist Dr He Jiankui announced that he had created the world’s first genome-edited babies to widespread condemnation.

He engineered mutations in human embryos that were later implanted into a woman, crossing an ethical boundary by altering the human germline, meaning the edits he made would also be passed on to future generations. Additionally, he was criticised for flouting normal safety procedures.
Jiankui claimed that he had disabled a gene called CCR5, offering protection against HIV. His critics pointed out that he could have also inadvertently caused mutations in other parts of the genome. Jiankui was jailed in China for three years at the beginning of 2020 and ordered to pay a three million yuan fine (£240,000 approx), his work a stark warning to everyone in the gene-editing world.
“This field is experimental and we are one ‘severe adverse event’ from the entire effort being frozen,” Urnov says. “The painful thing for me and for tens of thousands of folks like me who have spent 40 years building human genetic engineering to treat disease, you know, this technology’s now tainted with the concept of designer babies.
“We have 250 million people on planet Earth with genetic disease. We should not be talking about designing anyone. We should be putting all of our attention to the fact that there are hundreds of millions of our fellow human beings that have had their fate handed to them on genetic platter,” he adds.
There are other challenges to overcome, too. One of the major criticisms of Jiankui’s work stems from the fact that gene editing is not yet so precise that scientists haveabsolute faith that any edit only affects the part of the genome being targeted. There can be so-called ‘off-target’ effects: unintended genetic modification that occurs elsewhere on the target genome. A worst-case scenario in clinical terms might be ‘genotoxicity’, where an off-target effect causes DNA damage that could lead to cancer.
For this reason, what’s known as the ‘delivery challenge’ of CRISPR is a major focus of research, both at the IGI and beyond.

“We can only gain confidence in the safety of these procedures by performing clinical trials,” says Dr Ross Wilson, the IGI’s director of therapeutic delivery. “We are not so hubristic to think that we have the ability to forecast every possible outcome when a new therapeutic procedure is attempted, which is why these trials are being performed methodically and without haste.
"Once we have confidence that people’s lives are being saved or transformed for the better, without incurring unwanted outcomes, the technology can be moved into other applications, reducing risks of heart disease, for example.”
There are ways to offset this risk of unintended consequences of gene editing. A patient’s own cells can be sent to the lab for ‘trial editing’, giving an informed look at what is likely to happen inside that patient’s body when they are dosed.
CRISPRoff technology is also under development. This tool allows researchers to target the epigenome, rather than the genome itself. That is, scientists can turn off a particular gene without cutting a strand of DNA by instead targeting the proteins and other molecules that attach themselves to DNA and control when that gene is switched on or off. Because the genome itself is untouched, researchers expect the risk of unwanted effects to be lower.
“The pandemic taught us that the public has a major craving for things to be declared ‘safe’ or ‘unsafe’, but in reality it’s all about the balance between risk and benefit,” says Wilson. “That ratio looks extremely promising for CRISPR technology, and it improves each year, so the future is bright for therapeutic genome editing.”
Could CRISPR create a health inequality?
Doudna’s dream for CRISPR is to make it “the standard of medical care”. For that to happen, one more thing needs to be addressed, and it’s arguably more complex than any technical hurdle: the cost of treatment.
Gene editing is, or could be, a great leveller in healthcare. But like all experimental treatments, it is research-heavy, labour-intensive and expensive. One of Doudna’s fears is that it will become a boutique technology, available only to those who can afford it. This, she says, would not only exacerbate the health gap that already exists between rich and poor, but also create a new kind of health inequality: a gene gap.
The IGI is a non-profit, funded publicly and via philanthropy. Its staff talk of their work not just in technological terms but societal ones too, focused on how to maximise the reach of the technology.
“It’s a major problem,” Urnov says. “In the US, [some of] these medicines are sold for $2m, but European countries have refused to even licence them. You have a surreal situation where parents in Europe, whose children have these severe diseases, start GoFundMe campaigns to be able to pay American prices.
"We have this gap between the fact that this technology is rapidly expanding in its utility and we are struggling, frankly, with how to make it equitable and affordable.”
Add to that the issue of health justice, the fact that if you’re born with an inherited condition, an affordable cure may be possible if enough people have the same illness. That would make it economically viable for pharmaceutical companies to invest in the research to develop new treatments.
If you’re born with a rare genetic mutation, that may not be possible. “There is this horrific gap between our ability to read that person’s DNA and say, ‘Yes, this is the mutation that killed your mom and will kill you, I’m sorry to say’, and actually developing a treatment that would help that person. Developing such personalised cures has essentially no commercial value. Nobody will ever make money,” says Urnov.
Lovell-Badge agrees. “The cost is a problem for it becoming really useful for public health,” he says. “[We need to] start off from the very beginning thinking, ‘How can we do this in a way that’s going to be more affordable?’ Then you approach the problem in a different way.”
Unlike so much of the biotech industry, addressing this issue is a cornerstone that the IGI was built on – not just developing novel treatments, but creating scalable pipelines for discovery, testing and rollout.
“Our mission really has to be ensuring that technology benefits everyone,” Doudna says. “That was the impetus for the Innovative Genomics Institute in the first place. Many institutes, many companies, many academic labs are now developing gene editing, but not with an eye towards controlling cost and doing the science with a focus on public access to that technology. That’s really our purpose.”
The genetic revolution is coming. After pioneering the technology, Doudna is adamant that when it arrives, it’s available to everybody. As more than one of her colleagues tells us, that’s just in her DNA.
- This article first appeared inissue 367ofBBC Science Focus Magazine–find out how to subscribe here
Read more about DNA:
