What’s the difference between a headache and a migraine?
Headache is a neurological symptom, the underlying cause needs to be established. Migraine is a genetic, neurological condition often causing headache, but is also associated with many other symptoms including heightened sensitivity to light, sound, movement and smells, as well as dizziness, brain fog, abdominal pain, speech difficulties, visual disturbances, nausea, vomiting, fatigue and irritability. But this list is not exhaustive.
Migraine is a spectrum condition so some people have infrequent, mild attacks, while others have more severe, frequent episodes. Some suffer daily impact from the effects of migraine on their brain.

What happens during a migraine?
During migraine attacks, neurochemicals trigger a wave of electrical depolarisation at cell surfaces, known as ‘cortical spreading depression’, which spreads out over the brain. The effects of neurochemical disturbances may vary from person to person, from attack to attack, and throughout a person’s life.
‘Aura’ are neurological disturbances during the hour before the headache hits, and affect about a third of sufferers. Aura are often visual with zigzag lines, flashing lights, blurred vision or blind spots.
In the next phase, symptoms such as headache, ‘brain fog’ and fatigue can occur. Cognitive problems are common. The vagus nerve, which runs from the brain to the gut, is also affected. This slows down the emptying of the stomach, which can lead to nausea and sometimes vomiting, and delays absorption of helpful medications and may prolong attacks.
Pain during a migraine attack may be felt anywhere on the head, neck or shoulders. Abdominal pain is common in children.
Read more about migraines:
- The cause of migraines could be in sight (quite literally)
- A diet rich in omega-3 could reduce migraines
- Instant Genius Podcast: Migraines with Dr Katy Munro
How can you manage a migraine?
People hunt for that one thing they can do to stop attacks. They eliminate certain foods, stop caffeine and alcohol, searching for the key to switch off attacks. Sadly, it is not that simple. But you can try to keep track of what changes in the 48 hours before an attack. Using a simple headache diary may help identify some things to control in future and limit attack impact.
Diagnosis is on the history of symptoms. A migraine family history helps confirm the diagnosis, but is not essential and often unknown for various reasons.
Effective treatment requires the right medication in the right place at the right time. When a migraine attack starts to roll, it gathers momentum much like a snowball rolling down a mountain. Treating early is crucial, and discussing with a GP or headache specialist which combination of medications will suit you is so important.
Often a simple anti-nausea medication with a painkiller will help if taken early enough, but it may be necessary to add in migraine-specific medications called triptans. There are seven currently available. If one does not suit you, try a different one. The effect of each varies from person to person. These should not be taken on more than 10 days in the month, as overuse of acute migraine medication aggravates the brain. Avoid codeine and opiates which can quickly worsen migraine.
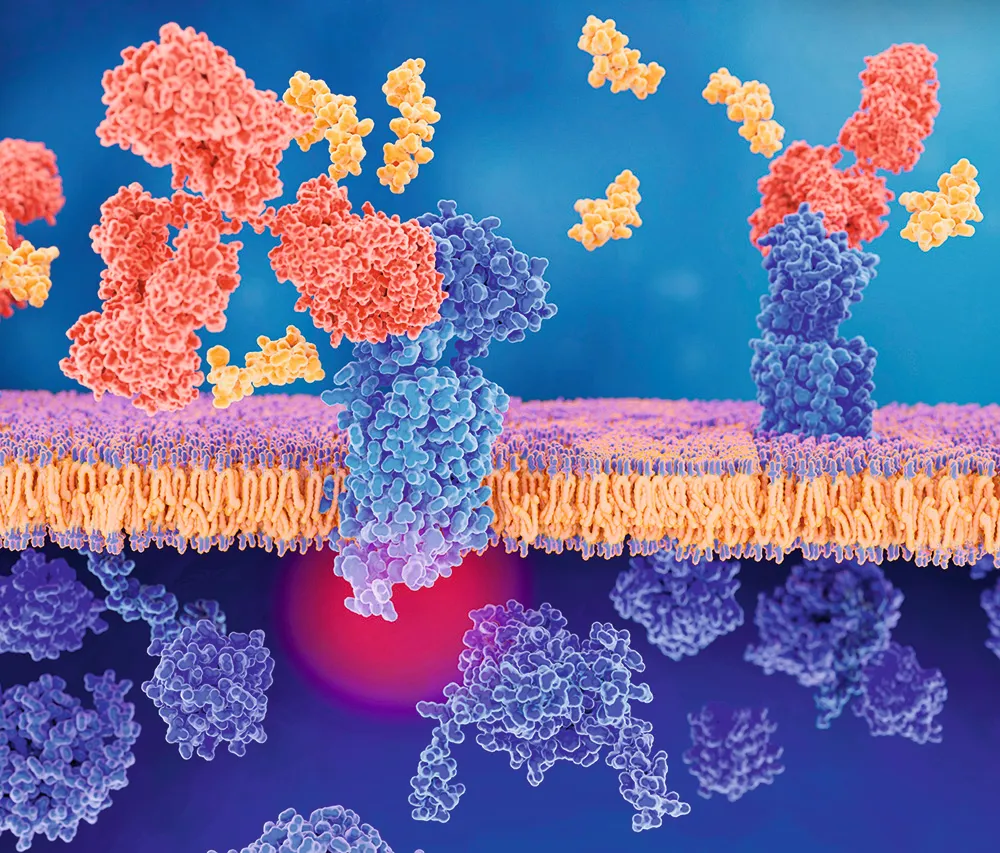
If you get more than about five attacks per month, explore preventive methods. There are many available, including supplements, medications, neuromodulation devices and injections. The newest are anti-Calcitonin Gene-Related Peptide (CGRP) self-administered injections.
CGRP is a pain neurochemical implicated in triggering attacks in some people. These monoclonal antibody injections block either CGRP neuropeptides, or receptors on cells. They can be extremely effective in reducing migraine attacks.
What causes migraine attacks?
Migraine genes set the brain to be less able to process sensory inputs and make the brain vulnerable to attacks. But that is not the whole story.
Epigenetics, the interaction of genes with our behaviours and environment, is important too. The more the brain is challenged by these stimuli, the more pain neurochemicals are produced. Migraine threshold theory suggests that combinations of changes irritate the brain and trigger attacks once pain neurochemicals reach a certain level.

‘Change’ is the key word. The migraine brain is more sensitive to internal body changes, such as blood sugar levels, sleep routines, hormones or stress, and external environment factors – light glare, strong visual patterns like stripes, stuffy air quality, and even weather.
Some things seem to be particularly likely to lead to attacks. Skipping meals leading to fluctuating blood glucose levels is one. Regular snacking may help. People with migraine are often sensitive to carbohydrates though, so low GI foods are preferable. Broken or extended sleep can aggravate attacks – this is especially hard for teenagers, who wake early for school but then lie in at weekends.
Hormones have a major role. Many teenagers have worsening attacks during the turbulent hormonal times of puberty, with growth spurts and menstrual cycles contributing. Many women find they have more attacks with their period and during perimenopause. Oestrogen levels change erratically before periods stop completely and often for some years afterwards.
Any type of change can lead to attacks worsening – a new job, moving house, travelling abroad. But so can stress reduction. ‘Let-down’ or weekend migraine attacks are commonly described – frustrating for people relaxing after a stressful time.
About the author - Dr Katy Munro
Katy is a GP headache specialist at the National Migraine Centre. She hosts the podcast Heads Up, and is the author of Managing Your Migraine (£9.99, Penguin Life).
Read more:
- Why do some people get migraines?
- What is pain?
- If the brain has no pain receptors, why do I get headaches?
- Is fish actually ‘brain food’?
To submit your questions email us at questions@sciencefocus.com (don't forget to include your name and location)